Quick Take
- Erections start with nerve signals that release nitric oxide.
- Nitric oxide boosts cGMP, relaxing smooth muscle and filling the penis with blood.
- Any disruption-vascular, nerve, hormone, or mind-can lead to erectile dysfunction.
- Typical checks include history, physical exam, blood tests, and sometimes ultrasound.
- First‑line treatments are lifestyle changes and PDE5 inhibitor pills; other options exist if needed.
When men have trouble getting or maintaining an erection, they are dealing with Erectile Dysfunction, a condition that affects millions worldwide. Understanding why an erection happens-and why it sometimes doesn’t-requires a look at nerves, blood vessels, hormones, and the brain. Below we break down the science in plain language, then map the most common reasons the system can fail.
How an Erection Happens: The Body’s Built‑In Pump
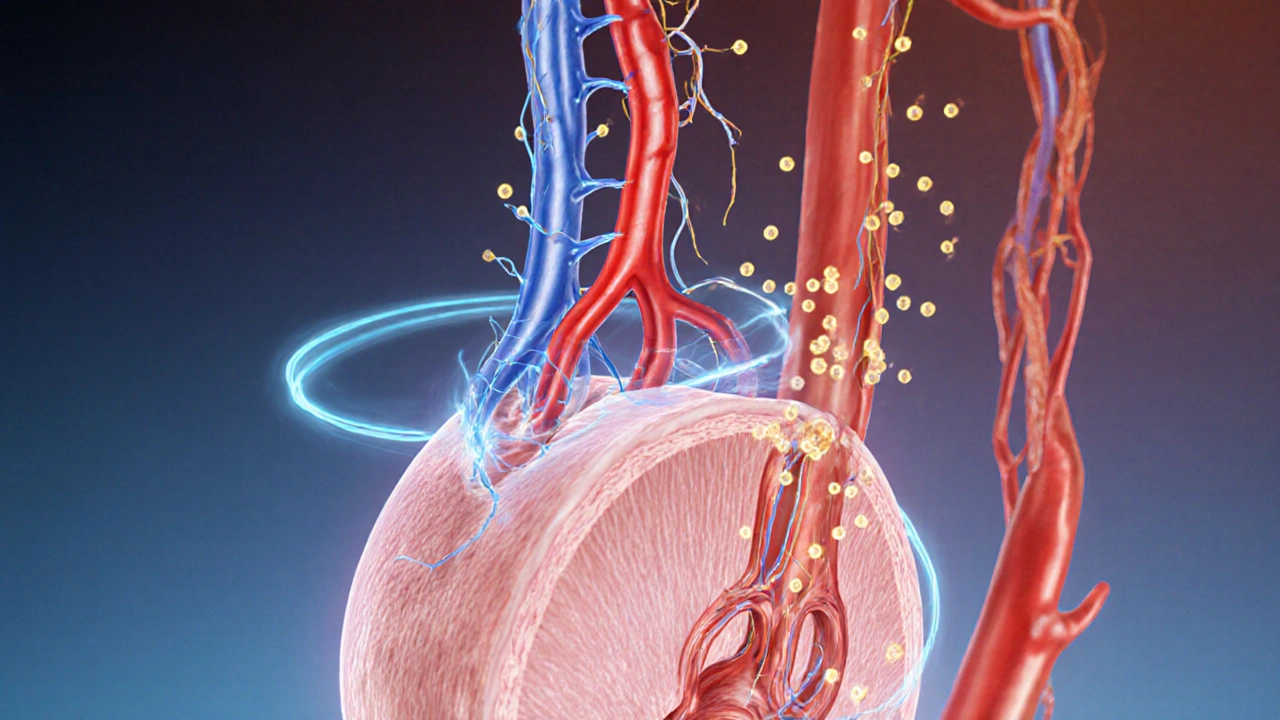
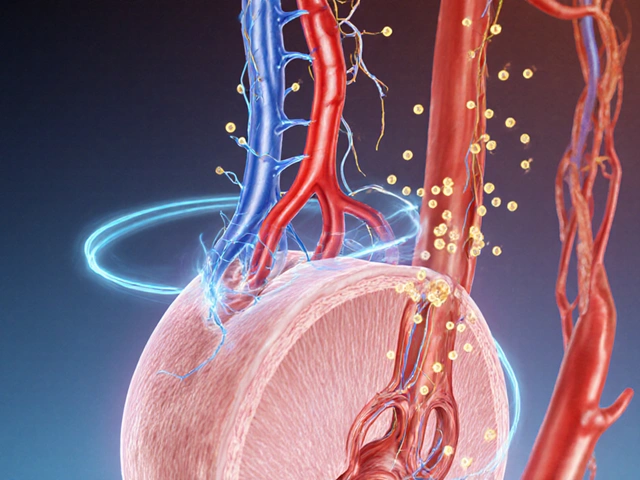
The penis contains three spongy columns of tissue. Two of them, the corpora cavernosa, sit side by side on the top; the third, the corpus spongiosum, runs along the underside and houses the urethra. When sexual arousal kicks in, the brain sends signals down the spinal cord to the pelvic nerves. Those nerves release Nitric Oxide (NO) into the erectile tissue.
NO does a very specific job: it activates an enzyme called guanylate cyclase, which turns GTP into cGMP. cGMP tells the smooth‑muscle cells lining the arteries to relax. When these tiny muscle fibers loosen, the arteries that feed the corpora cavernosa dilate, allowing a rush of blood to fill the cavernous spaces. At the same time, the veins that normally drain the penis are compressed, trapping the blood and creating rigidity.
Think of it like a balloon: the inflating air (blood) enters, the walls (smooth muscle) soften, and the exit valve (veins) is pinched shut, keeping the balloon firm.
The Hormonal and Psychological Layer
Even if the vascular engine works perfectly, the process can stall without the right hormonal backdrop. Testosterone fuels libido and helps maintain the health of the nerves and vessels involved in erection. Low testosterone levels can blunt desire, making the brain less likely to launch the NO cascade.
Beyond hormones, the mind plays a starring role. Stress, anxiety, depression, or relationship tension can interrupt the brain’s “go” signal. In those cases, the nerves either don’t fire enough NO or the brain actively sends a “stop” message, leading to a functional form of erectile dysfunction often labeled psychogenic.
When the System Breaks: Main Causes of Erectile Dysfunction
Doctors sort the reasons into four broad buckets. Each bucket reflects a different point where the chain reaction can be disrupted.
| Cause Category | Key Mechanism | Typical Signs | Common Triggers |
|---|---|---|---|
| Vascular | Reduced blood inflow or increased outflow | Hard to achieve firmness, especially in the morning | Heart disease, diabetes, smoking, high cholesterol |
| Neurogenic | Impaired nerve signaling | Occasional erections (e.g., nocturnal) but not during sex | Spinal cord injury, multiple sclerosis, pelvic surgery |
| Hormonal | Low testosterone or hormonal imbalance | Reduced desire, fatigue, loss of facial/body hair | Pituitary disorders, aging, certain medications |
| Psychological | Brain‑level inhibition | Marked anxiety about performance, sudden onset | Stress, depression, relationship problems |
Other contributors include medications (especially antihypertensives, antidepressants, and some prostate drugs) and lifestyle factors such as excessive alcohol or illicit drug use.

Diagnosing the Problem: What Doctors Look For
The first step is a frank conversation. Doctors ask about the onset, frequency, and any nighttime erections, which help separate physical from psychogenic causes. A physical exam checks the penis, testicles, and pulses in the groin and feet to gauge vascular health.
Blood tests often include:
- Glucose levels (to spot diabetes)
- Lipid panel (cholesterol and triglycerides)
- Testosterone concentration
- Thyroid‐stimulating hormone (TSH)
In tougher cases, a duplex ultrasound evaluates blood flow before and after a papaverine injection, revealing whether the arteries open enough.
Treatment Roadmap: From Lifestyle to Medication
Most men respond to the first line of care-changing habits and trying an oral pill.
- Lifestyle tweaks: quit smoking, limit alcohol, exercise 150minutes a week, manage weight, and control blood pressure.
- PDE5 Inhibitors (e.g., sildenafil, tadalafil): they block the enzyme that destroys cGMP, keeping the erection‑maintaining chemical around longer.
- Hormone therapy: testosterone replacement if labs confirm deficiency.
- Psychotherapy or sex counseling: effective for anxiety‑driven cases.
- Devices: vacuum erection devices or penile implants for refractory cases.
Each option has pros and cons, so a personalized plan based on the underlying cause works best.
Prevention: Keeping the System Running Smoothly
Because erectile function mirrors overall cardiovascular health, the same prevention steps apply.
- Eat a Mediterranean‑style diet rich in fruits, vegetables, whole grains, and omega‑3 fatty acids.
- Maintain a healthy waistline-abdominal fat predicts vascular disease.
- Stay active: brisk walking, cycling, or swimming boost nitric oxide production naturally.
- Monitor blood pressure and cholesterol annually.
- Address mental health early; stress‑relief techniques like mindfulness can keep the brain’s “go” signal on track.
When you protect your heart, you protect your erections.
Key Takeaway
Understanding how blood, nerves, hormones, and thoughts work together helps demystify erectile dysfunction. Whether the issue stems from clogged arteries, nerve damage, low testosterone, or stress, a clear diagnosis points to targeted treatment-and many men regain normal function with relatively simple changes.

Frequently Asked Questions
Can a man have erections at night if he has erectile dysfunction?
Yes. Nocturnal erections suggest the vascular and nerve systems are working, pointing to a psychological cause. If night‑time erections are missing, the problem is likely physical.
How long does it take for PDE5 inhibitors to work?
Sildenafil and vardenafil usually work within 30-60 minutes, while tadalafil can start in 15 minutes and lasts up to 36 hours.
Is low testosterone the main reason for erectile dysfunction in older men?
Low testosterone can lower libido, but vascular disease is more common in older adults. A blood test helps separate the two.
Can lifestyle changes reverse erectile dysfunction?
In many cases, yes. Quitting smoking, losing weight, exercising, and managing diabetes can improve blood flow enough to restore erections.
Are vacuum erection devices safe?
They are FDA‑approved and safe for most men. The main downside is occasional bruising or a feeling of reduced spontaneity.