When a pharmacist hands you a generic pill instead of the brand-name version, it’s not just a cost-saving trick-it’s a clinical decision backed by science, regulation, and careful communication. In the U.S., 97% of prescriptions filled are for generic drugs, saving the healthcare system over $400 billion a year. But behind every generic substitution is a conversation-often quiet, sometimes urgent-that happens between the pharmacist and the prescriber. This isn’t about swapping pills. It’s about ensuring safety, adherence, and trust.
Why Pharmacists Even Need to Talk to Prescribers
You might think if a generic is approved by the FDA, it’s automatically interchangeable. But that’s not always true. The FDA’s Orange Book, updated yearly, lists which generics are therapeutically equivalent to brand-name drugs. Most get an ‘A’ rating-meaning they’re bioequivalent and safe to swap. But about 7% get a ‘B’ rating, and those need extra scrutiny. Some drugs have a narrow therapeutic index-tiny changes in dose can mean the difference between healing and harm. Warfarin, levothyroxine, and phenytoin fall into this category. Even if a generic is technically equivalent, a prescriber may have chosen the brand for a reason: a patient’s history, a previous reaction, or a subtle difference in absorption. That’s why pharmacists don’t just swap and go. They check the prescription, review the patient’s record, and if anything seems off, they call the prescriber.When a ‘Do Not Substitute’ Flag Gets Raised
About 15% of prescriptions include a ‘dispense as written’ (DAW) instruction. That means the prescriber doesn’t want the pharmacy to substitute, even if a generic exists. Why? In 68% of these cases, it’s not because they distrust generics-it’s because they’ve seen something specific in the patient’s history. Maybe the patient had a seizure after switching from one brand to another. Maybe they’re on a complex regimen and stability matters more than savings. Pharmacists don’t ignore these flags. They respect them. But they also don’t let them go unexamined. If a patient is paying $300 for a brand-name drug when the generic costs $12, and there’s no documented clinical reason to avoid substitution, the pharmacist will reach out. Not to argue. To ask: Is this truly necessary?It’s Not Just About the Active Ingredient
Many people assume generics are identical to brand-name drugs. They’re not. They contain the same active ingredient, yes-but the fillers, dyes, and coatings can be different. For most people, that doesn’t matter. But for someone with a rare allergy to corn starch, lactose, or a specific dye, those inactive ingredients can trigger a reaction. According to the A-SMEDS guide, about 8.7% of substitution issues stem from these differences. A pharmacist might notice a patient’s allergy history and realize the generic they’re about to dispense contains a dye the patient reacted to last year. That’s not a theoretical risk. That’s a real, documented event. So they call the prescriber-not to delay care, but to prevent harm.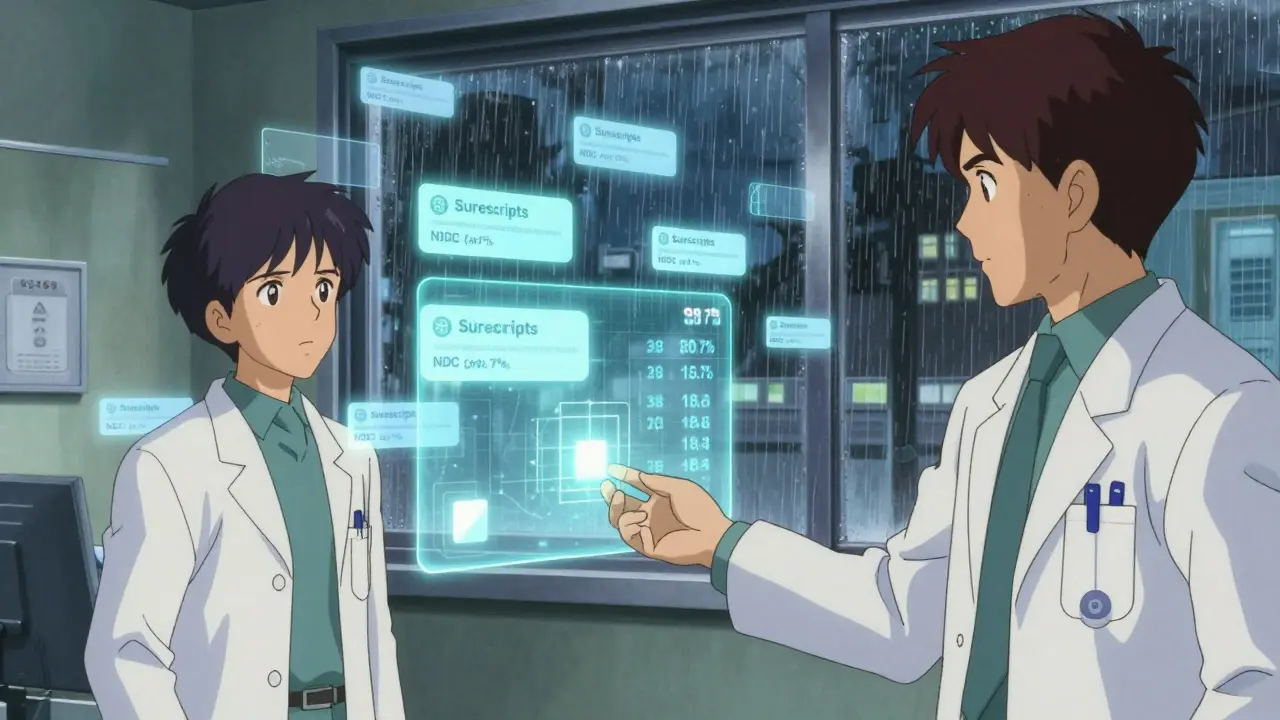
How Pharmacists Make Their Case
A good pharmacist doesn’t say, “The generic is cheaper.” They say, “The generic has the same bioequivalence profile as the brand, with 98.7% of approved generics falling within 95-105% of the reference drug’s absorption rates.” They cite the FDA’s Orange Book. They reference the 2018 Shrank study showing a 12.4% improvement in adherence with generics. They mention that patients on generics had 28.6% fewer medication non-adherence events and 15.2% fewer hospitalizations. They use tools built into electronic health records. Systems like Surescripts let pharmacists send a secure message with the generic’s NDC code, the Orange Book rating, and a link to the FDA’s Product-Specific Guidance for that drug. The prescriber gets it in seconds. The response rate? 82.4% acceptance when pharmacists use this structured approach. Without it? Only 57.3%.What Gets in the Way
Not every prescriber is open to the conversation. A 2023 survey found that 37.6% of prescribers still worry about generic efficacy-especially for inhalers, topical creams, or complex extended-release tablets. Some think, “If it worked with the brand, why change it?” But that’s not evidence-based. It’s habit. Time is another barrier. Pharmacists report having just 2.3 minutes per prescription to verify, counsel, and document. That’s not enough to dig into complex cases-unless they have the right tools. AI-powered platforms like PharmAI’s Generic Substitution Assistant are helping. Adopted by nearly 30% of chain pharmacies, these tools cut communication time by 42% and boost recommendation accuracy from 76% to 94%.
Documentation Isn’t Optional
If a pharmacist recommends a generic and the prescriber agrees, that decision must be documented. Not just in the pharmacy system-but in the patient’s medical record. CMS requires this for Medicare Part D. The American Medical Association and American Pharmacists Association agree on what needs to be recorded: the date and time of the conversation, the method used (phone, secure message), the prescriber’s name, the specific recommendation, and the outcome. Pharmacies that follow these standards see 27.5% fewer medication errors and 18.3% higher patient satisfaction. Why? Because when everyone knows what was decided, there’s no confusion later. No “I thought I was getting the brand” or “Why did my pill look different?”The Bigger Picture: Value-Based Care
This isn’t just about saving money. It’s about better care. Over 60% of Accountable Care Organizations now include pharmacist-led generic optimization in their quality metrics. Why? Because adherence drives outcomes. And generics improve adherence. The 2022 Inflation Reduction Act, effective January 2025, expands pharmacists’ role in Medicare Part D. More patients will get access to medication therapy management services-where pharmacists proactively review prescriptions, suggest generics, and coordinate with prescribers. That’s 21.3 million Medicare beneficiaries who could benefit from better communication. The FDA is also preparing to update the Orange Book with real-world data on how generics perform outside the lab. And the CDC is launching a Generic Medication Safety Network in late 2024, which will give pharmacists near-real-time alerts if a generic version of a drug shows unexpected side effects.It’s a Partnership, Not a Transaction
The best pharmacist-prescriber relationships aren’t built on authority. They’re built on trust. When a pharmacist calls with data, not doubt, and offers a solution-not just a complaint-the prescriber listens. When the pharmacist says, “I checked the Orange Book, the patient has a corn allergy, and the generic we’re considering has no lactose,” that’s not interference. That’s expertise. Generic substitution isn’t about cutting corners. It’s about making smarter choices. And when pharmacists communicate clearly, confidently, and with evidence, they don’t just save money-they save lives.Can pharmacists substitute generics without talking to the prescriber?
Yes, in 49 states, pharmacists can substitute a therapeutically equivalent generic unless the prescriber has marked ‘do not substitute’ or ‘dispense as written.’ But even when not legally required, many pharmacists still contact the prescriber for high-risk drugs like warfarin, levothyroxine, or medications with narrow therapeutic indexes. Patient safety always comes first.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generics to meet strict bioequivalence standards: their absorption rates must fall within 80-125% of the brand-name drug’s. In practice, 98.7% of approved generics stay within 95-105%, meaning they behave almost identically in the body. Studies involving over 12 million patients show no difference in clinical outcomes between generics and brand-name drugs for most conditions.
Why do some prescribers resist generic substitution?
Some prescribers worry about altered patient response, especially with complex drugs like inhalers or topical creams. Others fear patient complaints or think brand-name drugs are more reliable. But these concerns often stem from outdated beliefs. A 2023 Medscape survey found that 58% of prescribers still question generic efficacy-despite decades of evidence showing otherwise. Pharmacists help by sharing data, not opinions.
What if a patient has an allergy to an inactive ingredient in a generic?
That’s a common and valid concern. Generics can use different fillers, dyes, or binders. About 8.7% of substitution issues arise from these differences. Pharmacists check patient allergy histories before dispensing. If a generic contains a known allergen, they’ll either switch to another generic formulation or contact the prescriber to return to the brand. Patient safety overrides cost savings.
How do electronic health records help with generic communication?
Systems like Surescripts allow pharmacists to send secure, structured messages directly to prescribers with the generic’s NDC code, FDA equivalence rating, and cost comparison. This cuts communication time from over 8 minutes to under 3 minutes. It also ensures documentation is complete-94.8% of electronic records include full details, compared to just 63.5% with handwritten notes.
Will the Inflation Reduction Act change how pharmacists recommend generics?
Yes. Starting in 2025, the Inflation Reduction Act expands pharmacists’ role in Medicare Part D by allowing them to provide more comprehensive medication therapy management services. This includes proactively reviewing prescriptions, suggesting generics, and coordinating with prescribers-all part of a new focus on value-based care. Over 21 million Medicare beneficiaries will benefit from this change.