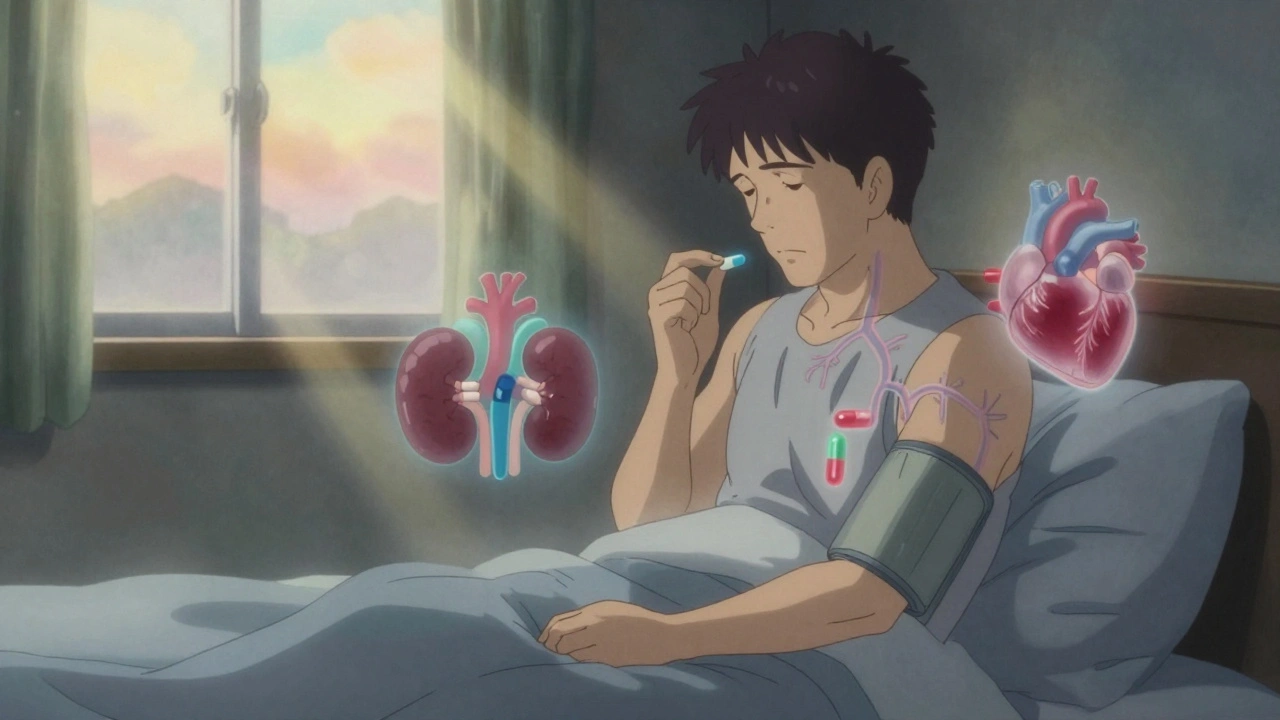
High blood pressure doesn’t always come with symptoms. That’s why it’s called the silent killer. But if you’ve been told you need medication to control it, you’re not alone. About half of all adults in the U.S. have hypertension, and many of them take one or more drugs every day to keep their numbers in check. The goal isn’t just to lower a number on a screen-it’s to protect your heart, brain, kidneys, and arteries from damage that can lead to stroke, heart attack, or kidney failure.
How Blood Pressure Medications Work
Blood pressure meds don’t work the same way. Each class targets a different part of how your body controls pressure. Some make your body get rid of extra salt and water. Others relax your blood vessels. Some slow your heart down. The right one-or combination-depends on your age, race, other health conditions, and even how your body reacts to drugs.
Doctors usually start with one of four main types: thiazide diuretics, calcium channel blockers, ACE inhibitors, or ARBs. These are backed by decades of research showing they reduce serious health events. If one doesn’t work well enough, they add another-not just more of the same, but a different kind. About 70% of people need two or more pills to reach their target.
Main Types of Blood Pressure Medications
- Thiazide diuretics (like hydrochlorothiazide): These help your kidneys flush out extra sodium and water. Less fluid in your blood means lower pressure. They’re often the first choice, especially for older adults and Black patients, because they’ve been proven to cut stroke risk in large studies.
- Calcium channel blockers (like amlodipine): These stop calcium from entering the muscle cells in your blood vessels, making them relax. Amlodipine is one of the most prescribed pills in the U.S. because it works well, has few side effects for most people, and doesn’t mess with blood sugar or cholesterol like some other drugs.
- ACE inhibitors (like lisinopril): These block a chemical that tightens blood vessels. They’re especially good for people with diabetes, heart failure, or kidney disease because they protect the kidneys. But about 1 in 5 people get a dry, annoying cough from them.
- ARBs (like losartan): These do almost the same thing as ACE inhibitors but block the effect at a different point. They don’t usually cause the cough, so they’re often used when someone can’t tolerate an ACE inhibitor.
- Beta-blockers (like metoprolol): These slow your heart rate and reduce how hard your heart pumps. They’re not first-line for most people anymore, but they’re essential if you’ve had a heart attack, have heart failure, or have a fast heartbeat. They can make you tired or give you cold hands and feet.
Other types exist for more complex cases: alpha-blockers, vasodilators, aldosterone blockers, and direct renin inhibitors. These are usually added when standard options aren’t enough-or when you have other conditions like severe kidney disease or adrenal tumors.
Common Side Effects You Should Know
Side effects aren’t rare. In fact, they’re one of the main reasons people stop taking their meds. About half of patients quit within a year-not because they feel fine, but because the pill makes them feel worse.
- Diuretics can make you pee more, which is fine during the day but annoying at night. They can also lower potassium too much, leading to muscle cramps or irregular heartbeat. Some people get gout flares.
- Calcium channel blockers like amlodipine often cause swollen ankles, dizziness, or flushing. Less common but real: gums can grow larger, which is why good dental care matters.
- ACE inhibitors cause that dry cough in 10-20% of users. Rare but dangerous: angioedema-a sudden swelling of the face, lips, or throat. If that happens, stop the drug and get help immediately.
- ARBs have similar risks to ACE inhibitors but without the cough. Still, they can raise potassium levels and are absolutely not safe during pregnancy.
- Beta-blockers can hide signs of low blood sugar in diabetics. That’s dangerous. They may also cause depression, sleep problems, or make you feel sluggish.
- Alpha-blockers like doxazosin can make you dizzy when you stand up. That’s called orthostatic hypotension. It’s especially risky for older adults.
Some side effects are mild and fade after a few weeks. Others stick around. If you’re struggling with one, don’t just quit. Talk to your doctor. There’s almost always another option.
Safety Rules: What to Avoid
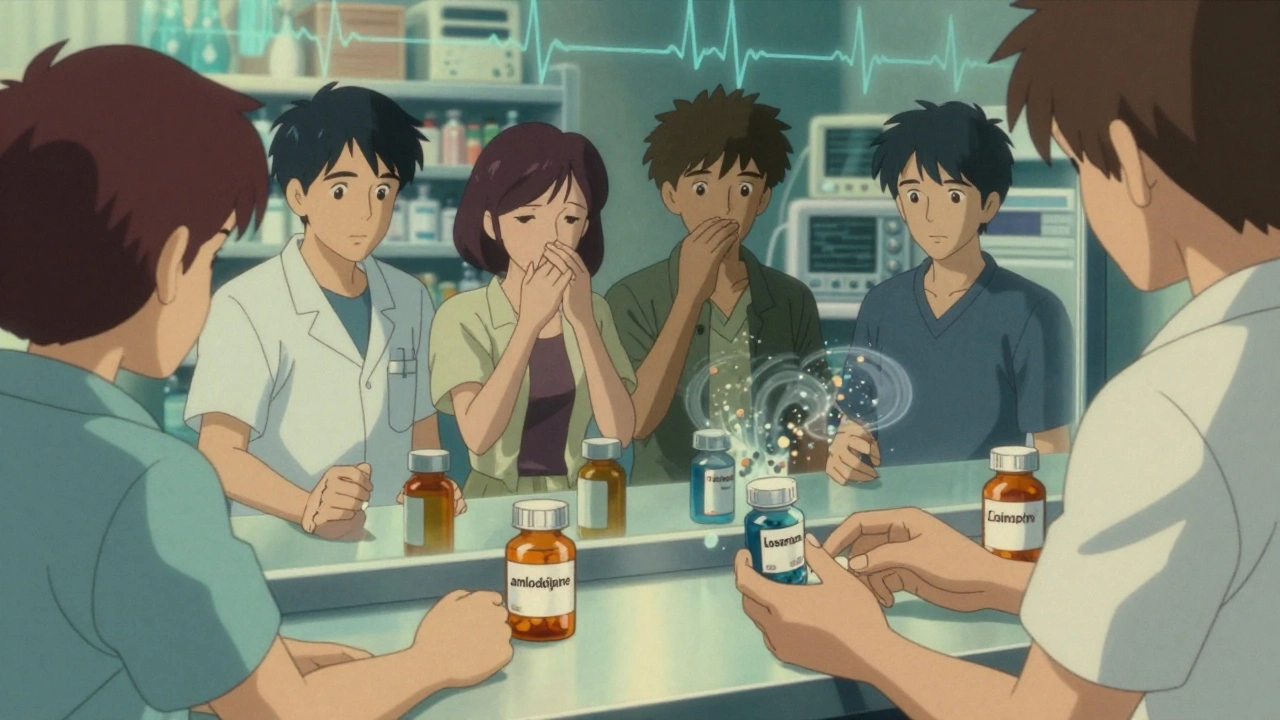
Not all drugs play nice together. Some combinations can be dangerous.
- Never combine ACE inhibitors and ARBs. This used to be tried for extra kidney protection, but studies show it increases the risk of kidney failure and dangerously high potassium without helping you live longer.
- NSAIDs like ibuprofen or naproxen can cancel out the effect of blood pressure meds and harm your kidneys, especially if you’re already on an ACE inhibitor or diuretic.
- Alcohol can make your blood pressure drop too low when mixed with meds, especially alpha-blockers or diuretics. It also makes dizziness worse.
- Pregnancy changes everything. ACE inhibitors, ARBs, and direct renin inhibitors can cause severe birth defects. Methyldopa and labetalol are safer choices during pregnancy.
- Older adults are more sensitive. Starting with half a dose is often smarter. Orthostatic hypotension can lead to falls, which are a leading cause of injury in seniors.
Who Gets Which Medication-and Why
There’s no one-size-fits-all. Your doctor picks based on your body and your risks.
- If you’re Black and have high blood pressure, thiazides or calcium channel blockers usually work better than ACE inhibitors or ARBs.
- If you have diabetes, ACE inhibitors or ARBs are preferred because they protect your kidneys.
- If you’ve had a heart attack, beta-blockers and ACE inhibitors are key-they help your heart heal and reduce the chance of another event.
- If you’re over 60 and have no other major health issues, a diuretic or calcium channel blocker is often the best first step.
- If you have kidney disease with protein in your urine, ACE inhibitors or ARBs are the gold standard.
For stage 2 hypertension (140/90 or higher), current guidelines say to start with two drugs right away. That’s not because one isn’t enough-it’s because waiting to add a second drug means more time with dangerous pressure levels.
Adherence: The Biggest Challenge
Medication only works if you take it. But hypertension has no pain, no fever, no visible signs. So why take a pill every day?
Studies show half of people stop their blood pressure meds within a year. Reasons? Side effects, forgetfulness, cost, or thinking, “I feel fine.” But your blood pressure isn’t asking how you feel. It’s quietly damaging your organs.
Here’s what helps:
- Use a pill organizer or phone reminders.
- Ask your doctor about combination pills-some brands put two drugs in one tablet, cutting your daily count in half.
- Get your blood pressure checked at home. Seeing your numbers improve can be motivating.
- Talk openly about side effects. There’s almost always a workaround.
What’s Next? The Future of Treatment
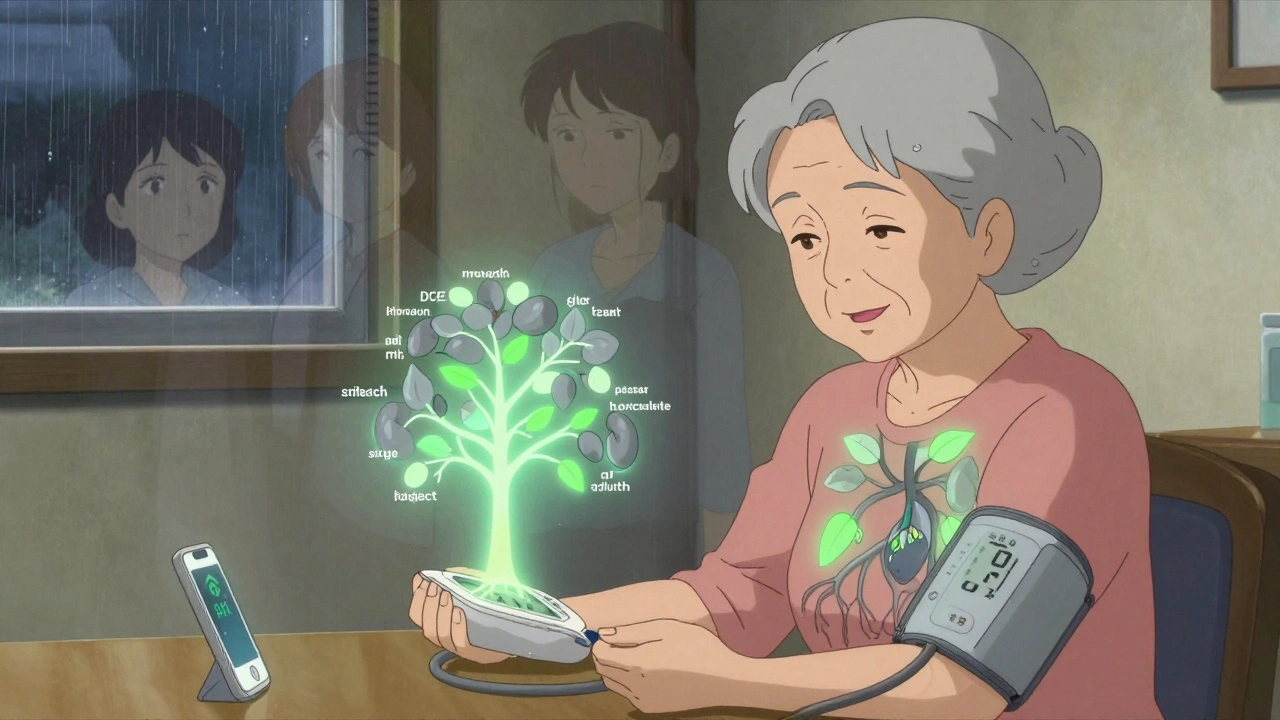
Research is moving fast. Doctors are starting to use genetic testing to guess which drug might work best for you-like whether you’re likely to get a cough from an ACE inhibitor or respond better to a calcium channel blocker. It’s not mainstream yet, but it’s coming.
Smart devices are helping too. Apps that remind you to take pills and sync with home blood pressure cuffs have been shown to improve adherence by 15-20%. That’s not just convenient-it’s life-saving.
And while we still rely on the same five main classes, new drugs are being tested for resistant hypertension-cases where even three or four pills don’t bring pressure down. These include drugs that target nerve signals in the kidneys or block specific hormones linked to stubborn high pressure.
For now, though, the best strategy is simple: know your numbers, take your meds as directed, and speak up when something doesn’t feel right. You don’t have to live with side effects. There’s always another option.
Can I stop taking blood pressure medication if my numbers are normal?
Only under your doctor’s supervision. Normal blood pressure on meds doesn’t mean the problem is gone-it means the meds are working. Stopping suddenly can cause a dangerous spike. Some people can reduce or stop meds after major lifestyle changes, but that’s a slow, monitored process-not a decision to make on your own.
Which blood pressure medication has the least side effects?
There’s no single answer. Amlodipine (a calcium channel blocker) tends to have fewer bothersome side effects for most people, especially compared to beta-blockers or diuretics. But side effects depend on your body. One person tolerates lisinopril fine; another gets a cough. It’s about trial and communication with your doctor.
Do blood pressure meds damage your kidneys?
Most protect your kidneys-especially ACE inhibitors and ARBs. But if you take NSAIDs like ibuprofen with them, or combine ACE inhibitors with ARBs, you can hurt your kidneys. Also, if your blood pressure drops too low due to overmedication, your kidneys can suffer. Monitoring and proper dosing prevent this.
Why do I need to take more than one pill?
High blood pressure is caused by multiple factors-fluid volume, blood vessel tightness, heart rate, hormone levels. One drug usually can’t fix all of them. Using two or three that work in different ways gives better control with lower doses of each, which often means fewer side effects.
Are natural remedies enough to replace blood pressure meds?
Lifestyle changes-like losing weight, cutting salt, exercising, and reducing alcohol-can lower blood pressure significantly. For some with mild hypertension, they might delay or reduce meds. But for most people with stage 1 or 2 hypertension, meds are still needed. Natural remedies aren’t proven to prevent strokes or heart attacks the way FDA-approved drugs are.
What to Do Next
If you’re on blood pressure medication:
- Take it at the same time every day-even if you feel fine.
- Keep a log of your home readings and bring it to appointments.
- Ask your pharmacist or doctor about potential interactions with supplements or OTC painkillers.
- If you’re having side effects, don’t suffer silently. There’s almost always a better fit.
- Get your potassium and kidney function checked at least once a year if you’re on ACE inhibitors, ARBs, or diuretics.
If you’re not on meds but have high blood pressure:
- Get checked regularly-don’t wait for symptoms.
- Start with lifestyle changes, but don’t delay meds if your doctor recommends them.
- Know your numbers. Systolic over 130 or diastolic over 80 means action is needed.
High blood pressure doesn’t care if you’re busy, tired, or scared. But with the right meds, monitoring, and support, you can live a long, healthy life-even if you need pills to do it.