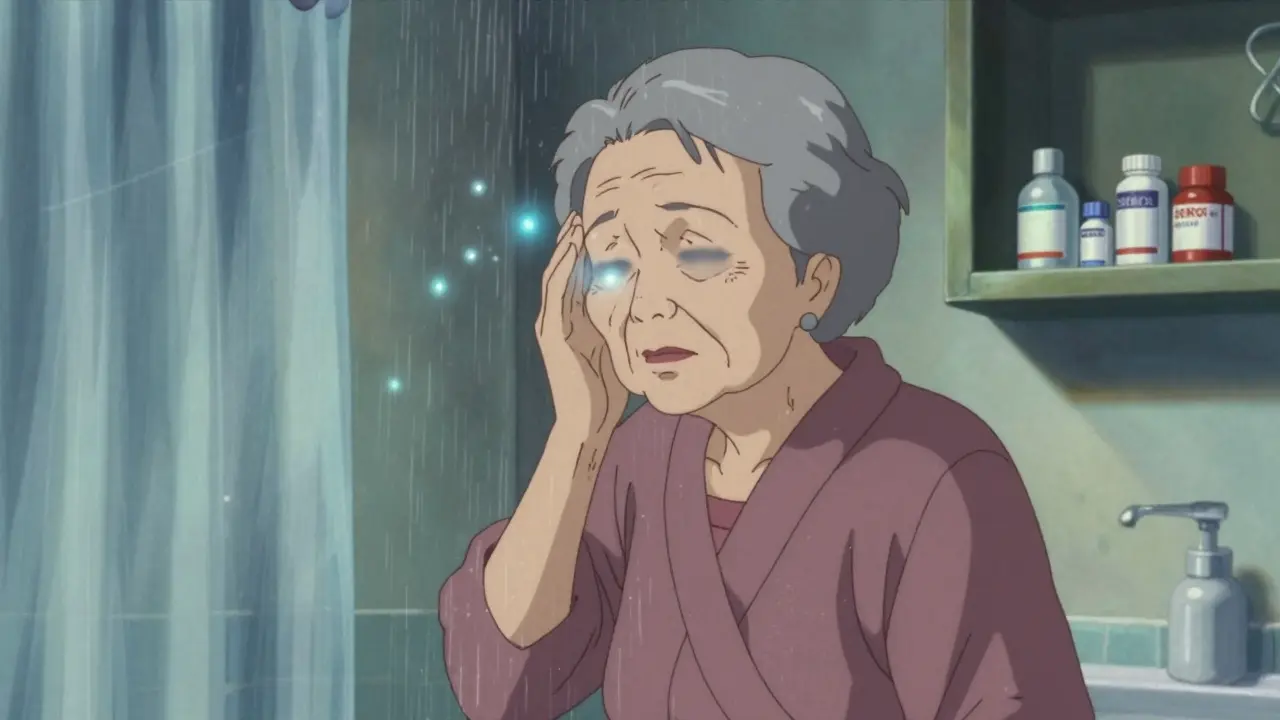
When doctors prescribe SSRIs to older adults for depression or anxiety, they’re often thinking about mood improvement. But there’s a quiet, dangerous side effect hiding in plain sight: hyponatremia - low sodium in the blood - and the falls that follow. It’s not rare. About 1 in 5 Americans over 65 are on these meds, and for many, the first sign isn’t sadness or fatigue - it’s stumbling on the stairs or feeling dizzy in the shower.
Why Older Adults Are at Higher Risk
Your body changes as you age. Less water. Slower kidneys. Hormones that don’t talk to each other like they used to. These aren’t just quirks - they’re risk factors. SSRIs interfere with a hormone called ADH, which tells your kidneys how much water to hold onto. When SSRIs overstimulate ADH, your body starts retaining too much water. That dilutes your sodium. And when sodium drops below 135 mmol/L, you’ve got hyponatremia.It’s worse in older adults because they naturally have less total body water. A 70-year-old has about 50% less water than a 30-year-old. That means even a small amount of extra fluid can swing sodium levels dangerously low. And it doesn’t take long - most cases show up within two to four weeks after starting or increasing the dose.
The Silent Warning Signs
Hyponatremia doesn’t always scream for attention. In fact, 30-40% of older adults show no symptoms at all until it’s too late. But when it does show up, it often looks like aging - confusion, dizziness, weakness, unsteady walking. These aren’t just "getting older" symptoms. They’re red flags.And here’s the real danger: when your sodium drops, your balance goes with it. Dizziness isn’t just uncomfortable - it’s a fall waiting to happen. A fall can mean a hip fracture, hospitalization, loss of independence. Studies show SSRIs increase fall risk by up to 40% in seniors, and hyponatremia is a major driver. Yet, no study has directly measured the percentage of falls caused by low sodium. That gap matters. Because if we can’t see the connection clearly, we won’t act fast enough.
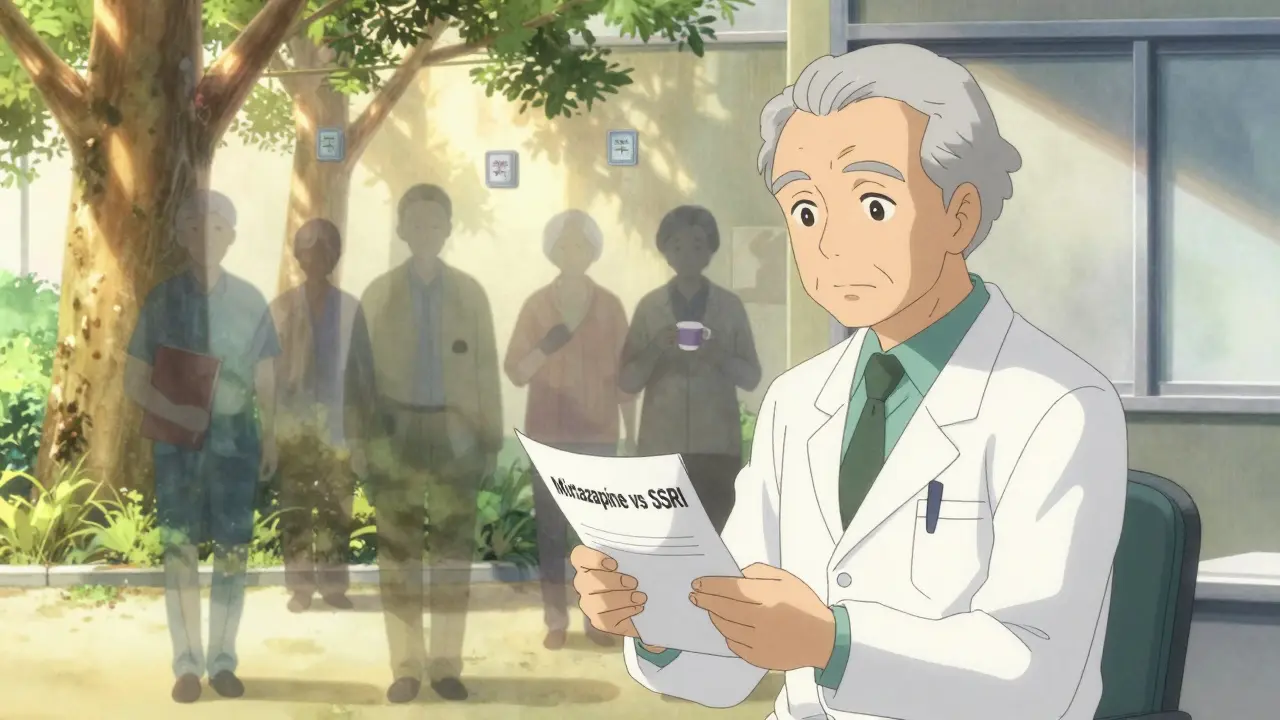
Which SSRIs Are Riskiest?
Not all SSRIs are created equal. Fluoxetine (Prozac) has the highest risk, with nearly 7 out of every 100 users developing hyponatremia. Sertraline and citalopram are close behind. Venlafaxine (an SNRI, not an SSRI but often grouped with them) is even riskier - over 5% of users develop low sodium.On the other end, mirtazapine (not an SSRI) has almost no link to hyponatremia. Bupropion (Wellbutrin) is another low-risk option. So if someone is 78, has a BMI under 20, takes a diuretic, and just started an SSRI - switching to mirtazapine might be safer than continuing.

The Thiazide Trap
Here’s a deadly combo: SSRIs + thiazide diuretics. This pair is like pouring gasoline on a fire. Thiazides - used for high blood pressure - make your kidneys flush out sodium. SSRIs make your body hold onto water. Together? They create a perfect storm. Studies show this combo increases hyponatremia risk by 24-27%. It’s so common, many elderly patients are on both without anyone connecting the dots.One 2023 study of Medicare patients found that nearly 1 in 10 older adults on SSRIs were also taking a thiazide. And in nearly half of those cases, no one checked their sodium levels. That’s not negligence - it’s systemic blindness.
What Should Be Done? Monitoring, But Not Just Testing
Doctors are told to check sodium before starting SSRIs and again at two weeks. That’s standard advice. But here’s the twist: a 2023 study found that even when this monitoring happened, it didn’t reduce hospitalizations. Why? Because checking sodium isn’t enough. You need to act.If sodium drops below 130, stop the SSRI. If it’s between 125 and 134, cut fluids and monitor closely. Below 125? That’s an emergency - hospitalization needed. But many clinics don’t have systems to act fast. A lab result comes back on Friday. The doctor is out Monday. The patient falls on Tuesday. The system breaks.
Some places are fixing this. Johns Hopkins Bayview Medical Center added three steps: baseline sodium test, two-week follow-up, and patient education about dizziness and weakness. Result? A 22% drop in ER visits for hyponatremia. Not perfect. But real.
What’s Changing Now?
The FDA updated SSRI labels in 2022 to highlight hyponatremia risk. The American Geriatrics Society now lists SSRIs as potentially inappropriate for seniors with existing low sodium or risk factors. And a new AI tool launched in 2024 flags high-risk combinations - like fluoxetine + hydrochlorothiazide - and prompts automatic sodium testing.Still, the big question remains: if we catch hyponatremia early, why do people still end up in the hospital? That’s why the NIH is funding a $2.8 million study starting September 2024 to find out what actually works. Until then, the best approach is simple: know the risk, know the signs, and don’t wait for a fall to happen.
Alternatives That Work
Not everyone needs an SSRI. For mild to moderate depression, talk therapy - especially cognitive behavioral therapy - works just as well in older adults. And it doesn’t lower sodium. But access is a problem. Many seniors can’t drive to appointments. Home-based therapy or telehealth options are scarce.Mirtazapine is a strong alternative. It helps with sleep and appetite, which many older adults struggle with. Bupropion can help with energy and motivation. Neither carries the hyponatremia risk. If someone has a history of falls, low BMI, or takes a diuretic - switching to one of these might be the safest move.
What You Can Do
If you or a loved one is on an SSRI:- Ask for a baseline sodium test before starting - and a repeat at two weeks.
- Ask if any other meds (especially diuretics) are being taken - and whether they’re necessary.
- Watch for dizziness, confusion, or trouble walking - even if it seems "just part of aging."
- Report any falls, even minor ones, to your doctor. They’re not accidents - they’re signals.
- Ask about alternatives like mirtazapine or therapy if you’re at high risk.
Depression is real. But so is the cost of treating it with the wrong tool. We don’t need to choose between mood and safety. We need better choices.
Can SSRIs cause falls in older adults?
Yes. SSRIs increase fall risk in older adults, primarily through a side effect called hyponatremia - low sodium in the blood. This causes dizziness, confusion, and poor balance, which can lead to falls. Studies show a 30-40% higher fall rate in seniors on SSRIs compared to those not taking them. While not every fall is caused by low sodium, it’s one of the most common and preventable triggers.
How do I know if my elderly parent has hyponatremia from an SSRI?
Symptoms are often subtle: unsteadiness when walking, sudden confusion, nausea, headache, or weakness. Many people don’t feel anything until the sodium level drops dangerously low. The only reliable way to know is a blood test. If your parent started an SSRI in the last month and is showing any of these signs, ask for a serum sodium test immediately.
Should all older adults on SSRIs get their sodium checked?
Yes - especially if they’re over 65, have a low body weight, take a diuretic, or have had a fall. Even if they feel fine, a sodium test before starting and again at two weeks can catch problems early. While one study found monitoring didn’t reduce hospitalizations, that was likely because follow-up actions weren’t taken. Testing alone isn’t enough - but testing + action saves lives.
Are there antidepressants safer than SSRIs for seniors?
Yes. Mirtazapine has almost no link to hyponatremia and often helps with sleep and appetite - common issues in older adults. Bupropion is another low-risk option, especially if energy and motivation are concerns. Psychotherapy, particularly CBT, is effective for mild to moderate depression and carries no physical risks. Talk to a geriatric psychiatrist about switching if your loved one is at high risk.
Why is the combination of SSRIs and thiazide diuretics so dangerous?
Thiazide diuretics make the body lose sodium. SSRIs make the body hold onto water. Together, they create a perfect storm: sodium drops while fluid builds up. This combo increases hyponatremia risk by over 25%. It’s one of the most common medication interactions in older adults - and one of the most preventable. Always ask if the diuretic is still needed, and whether a different blood pressure med might be safer.