Medication Side Effect Risk Calculator
Find out the estimated risk of sexual side effects from your medication. This tool uses clinical data to provide personalized risk assessment based on the medication class you're taking.
Results
What to do next
It’s not rare. In fact, it’s more common than most people realize. If you’re taking an antidepressant, antipsychotic, or even some blood pressure meds, there’s a very good chance you’re experiencing sexual side effects - and no one ever told you it might happen. You might be struggling with low desire, trouble getting or keeping an erection, delayed or absent orgasm, or pain during sex. And if you’re like most people, you didn’t bring it up with your doctor because you thought it was just something you had to live with.
Why This Happens - And Why It’s Not Your Fault
Many medications affect the chemicals in your brain that control sexual response. SSRIs like sertraline, fluoxetine, and paroxetine are the most common culprits. Between 58% and 70% of people taking these drugs report sexual side effects, according to Psychiatry Advisor (2023). That’s more than half. For men, it’s often trouble with erections or delayed ejaculation. For women, it’s usually low desire, trouble reaching orgasm, or painful sex. These aren’t psychological issues - they’re biological side effects of how the drug interacts with serotonin and other neurotransmitters. And here’s the twist: up to half of people with depression already have sexual problems before they even start medication. So when a doctor says, “Your libido’s low because you’re depressed,” it might be true - or it might be the pill. That’s why it’s crucial to track your symptoms before and after starting treatment.The Cost of Silence
Most people don’t talk about this. A 2022 survey by NAMI found that 73% of patients who had sexual side effects waited an average of 4.2 months before telling their provider. Why? Embarrassment. Fear of being judged. Belief that nothing can be done. But staying silent has real consequences. A 2003 national survey showed that 41.7% of men and 15.4% of women stopped taking their psychiatric meds because of sexual side effects. That’s not just discomfort - that’s treatment failure. When people don’t speak up, they’re not just risking their mental health. They’re risking their relationships, their self-esteem, and their long-term recovery. One patient on HealthUnlocked shared: “When my doctor switched me to bupropion after I mentioned sexual problems at our 6-week check-in, my sex life improved within 2 weeks and I’ve stayed on treatment for 18 months now.” That’s the power of speaking up - and being heard.What Good Counseling Looks Like
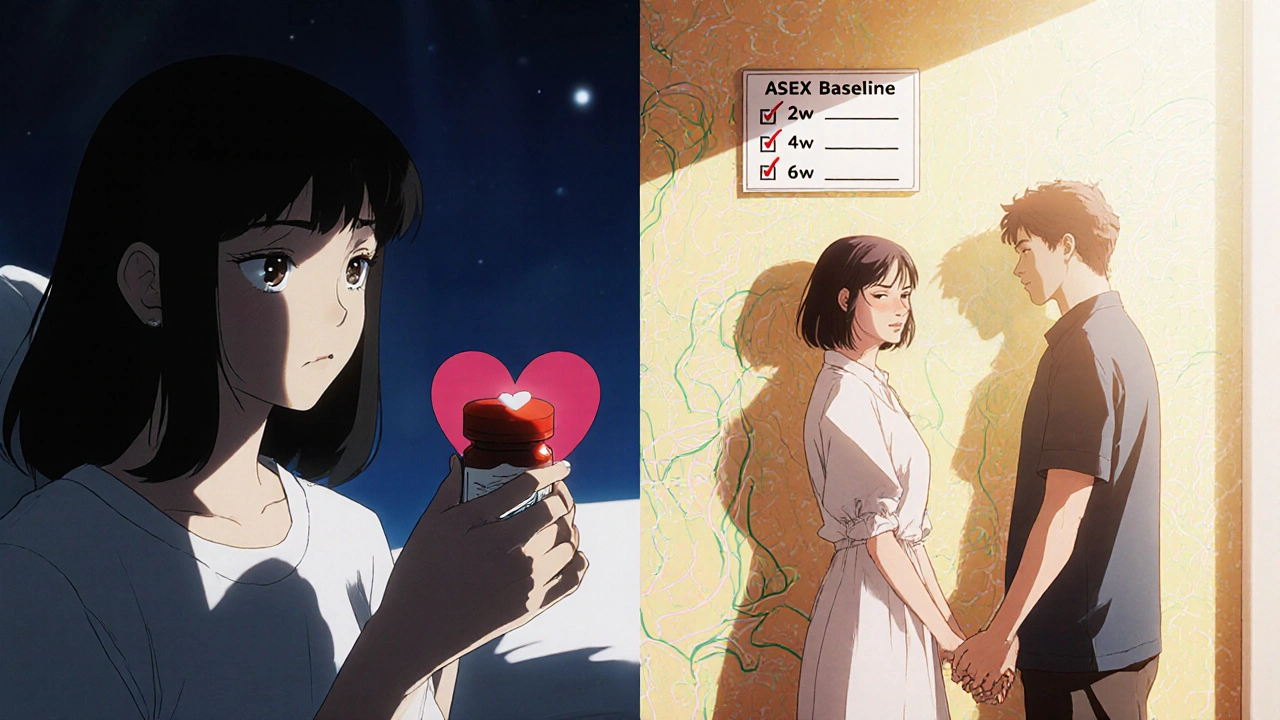
Good counseling doesn’t wait until you’re already suffering. It starts before you even take the first pill. Experts like Dr. Andrew C. Levine say: “Prior to prescribing an antidepressant, inform patients that it is possible, although not inevitable, that their sexual life will be affected.” That’s not scare tactics - it’s informed consent. Effective counseling includes four key steps:- Baseline assessment - Before starting medication, use a simple tool like the Arizona Sexual Experience Scale (ASEX). It takes less than 10 minutes and gives you a clear starting point.
- Clear communication - Your provider should tell you the exact risk for your specific drug. For example: “Fluoxetine causes sexual side effects in about 65% of users. Bupropion is much lower - around 7%.”
- Structured follow-up - Don’t wait for your next routine appointment. Check in at 2, 4, and 6 weeks. Ask: “How’s your sex life?” That’s it. No beating around the bush.
- Contingency plan - If side effects happen, what are your options? Know them ahead of time.
What Works - And What Doesn’t
There’s no one-size-fits-all fix, but several strategies have proven results:- Switching medications - Going from an SSRI to bupropion or mirtazapine works for 65-70% of people. Bupropion is especially good because it rarely causes sexual side effects - and may even improve desire.
- Dose reduction - Lowering the dose helps in 25-30% of cases. Sometimes, you can maintain mood improvement while reducing side effects.
- Drug holidays - Skipping your pill for 2-3 days before sex can help, especially with short-acting drugs like paroxetine. But there’s a 15% risk of relapse. Not for everyone.
- Adding sildenafil (Viagra) - Works well for erectile issues (55-60% success), but doesn’t help much with low desire or orgasm problems.
- Couples therapy - If the side effect has caused tension in your relationship, therapy can help. Success rate: about 50%.
And here’s a critical point: PDE5 inhibitors like Viagra are often misused. Many people take them without understanding their limits. They don’t fix low libido. They don’t fix delayed orgasm. They only help with blood flow to the penis. If your doctor prescribes one without explaining this, you’re being set up to fail.
Who’s Talking About This - And Who Isn’t
The truth? Many providers still avoid the topic. A 2021 JAMA Internal Medicine survey found that 64% of medical residents felt uncomfortable discussing sexual side effects. That’s not because they don’t care - it’s because they weren’t trained to do it well. And the gaps are worse for certain groups. LGBTQ+ patients report 28% fewer discussions about sexual side effects than heterosexual patients, according to a 2022 study in the Journal of Sexual Medicine. Women are also under-researched. Only 12% of clinical trials on sexual dysfunction specifically focus on female patients. But things are changing. The American Psychiatric Association now mandates routine sexual function checks in their 2022 depression guidelines. Major health systems are rolling out screening protocols. Telehealth companies like Ro and Hims now offer specialized services for medication-related sexual issues. And the FDA now requires clearer warnings in medication guides.
What You Can Do Right Now
If you’re on medication and experiencing sexual side effects:- Write down your symptoms - When did they start? How often do they happen? Are they worse at certain times of day?
- Ask your provider these questions:
- “Is this side effect likely from my medication?”
- “What are my options if this doesn’t improve?”
- “Can we try switching to a drug with lower sexual side effects?”
- “Are there non-medication strategies that might help?”
- Don’t assume it’s permanent - Most side effects are reversible. Sometimes just switching drugs is enough.
- Bring a partner - If you’re comfortable, invite them to the appointment. Relationship strain is part of this issue - and they deserve to be part of the solution.
What’s Coming Next
New treatments are on the horizon. A phase 3 clinical trial (NCT04891234) is testing a drug designed to block serotonin receptors that cause sexual side effects - without reducing antidepressant benefits. Results are expected in mid-2024. Meanwhile, apps like MoodFX now let you track mood and sexual function together, giving you real data to share with your doctor. Experts predict that within five years, checking for sexual side effects will be as routine as checking your weight or blood pressure. By 2030, if we keep improving how we handle this, we could cut medication discontinuation due to sexual issues by half. This isn’t about sex. It’s about dignity. It’s about being able to live fully while managing your mental health. You don’t have to choose between feeling better mentally and feeling connected in your body. With the right support, you can have both.Do all antidepressants cause sexual side effects?
No. While SSRIs like sertraline and fluoxetine cause sexual side effects in 50-70% of users, other antidepressants like bupropion and mirtazapine have much lower rates - around 5-10%. Bupropion is often chosen specifically because it’s less likely to affect libido or orgasm.
Can I just stop taking my medication if sex is affected?
Stopping abruptly can cause withdrawal symptoms or make your depression worse. Instead, talk to your provider. There are safer options: dose adjustments, switching medications, or adding treatments that help with side effects. Never stop without medical guidance.
Is it normal to feel embarrassed talking about this with my doctor?
Yes, it’s very common. But remember - your doctor has likely heard this from dozens of patients. The more you talk about it, the easier it gets. Providers who are trained in sexual health know how to respond with empathy and practical solutions. You’re not being weird - you’re being honest.
Can therapy help with sexual side effects from meds?
Yes, especially if the side effects have caused relationship stress, shame, or anxiety. Couples therapy or sex therapy can help you and your partner reconnect emotionally and physically. Studies show it improves outcomes in about 50% of cases where relationship strain is present.
Are there any new treatments coming soon?
Yes. A new drug targeting the 5-HT2C receptor is in phase 3 trials and could be available by 2025. It’s designed to reverse SSRI-induced sexual dysfunction without reducing the antidepressant effect. Apps that track mood and sexual function are also becoming more common, helping patients and providers make data-driven decisions.
Why don’t more doctors talk about this?
Many providers weren’t trained to discuss sexual health. A 2021 survey found that 64% of medical residents felt uncomfortable bringing it up. Time limits in appointments and lack of standardized protocols also play a role. But guidelines are changing - and patient demand is pushing systems to improve.
Does this only affect people on antidepressants?
No. Antipsychotics, blood pressure medications like beta-blockers, and even some hormonal treatments can cause sexual side effects. For example, antipsychotics that raise prolactin levels can lead to low desire and erectile problems. Always ask about potential side effects when starting any new medication.

