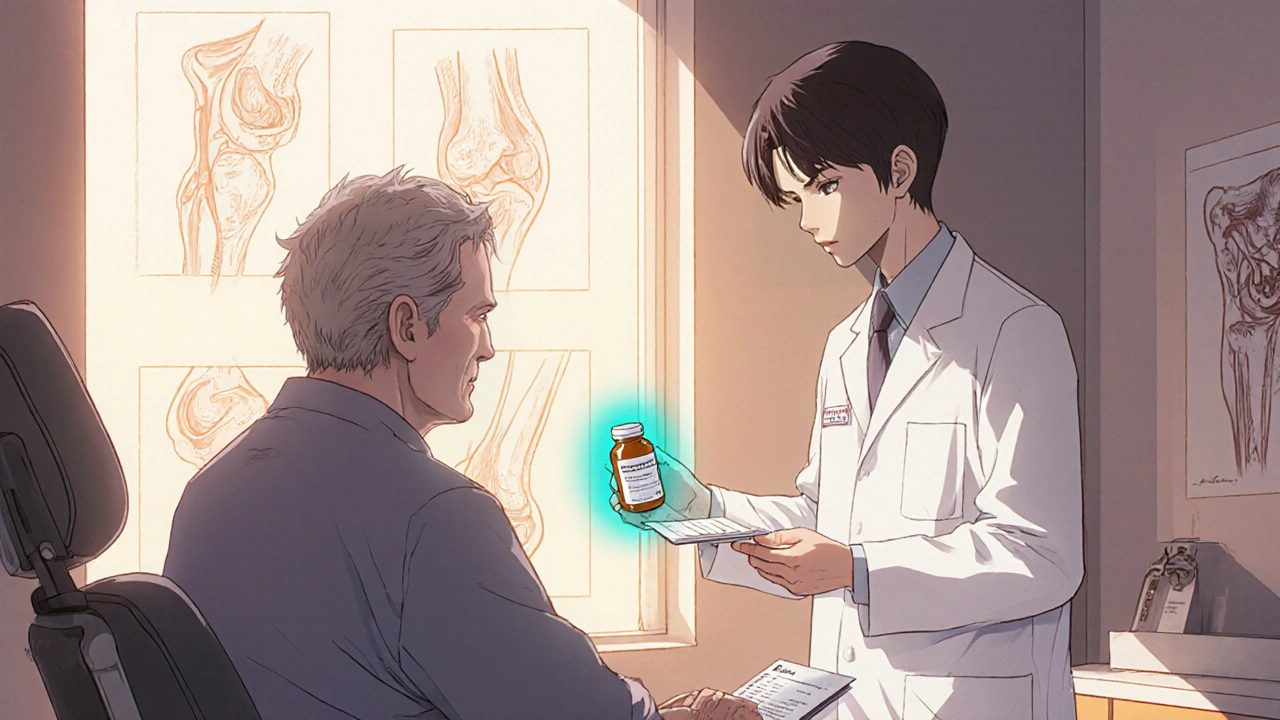
When it comes to protecting joints, Pentosan polysulfate is a prescription drug originally created for bladder pain, but doctors have been repurposing it to tackle a range of joint problems. In the last decade the molecule has moved from niche urology clinics into orthopaedic offices, physiotherapy rooms, and even some sports medicine practices.
How Pentosan Polysulfate Works
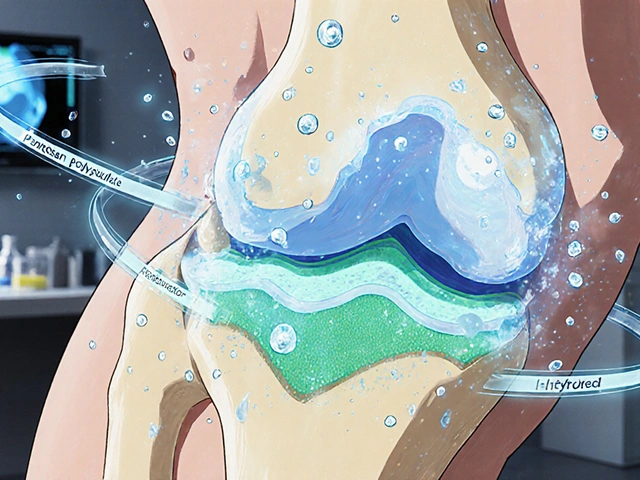
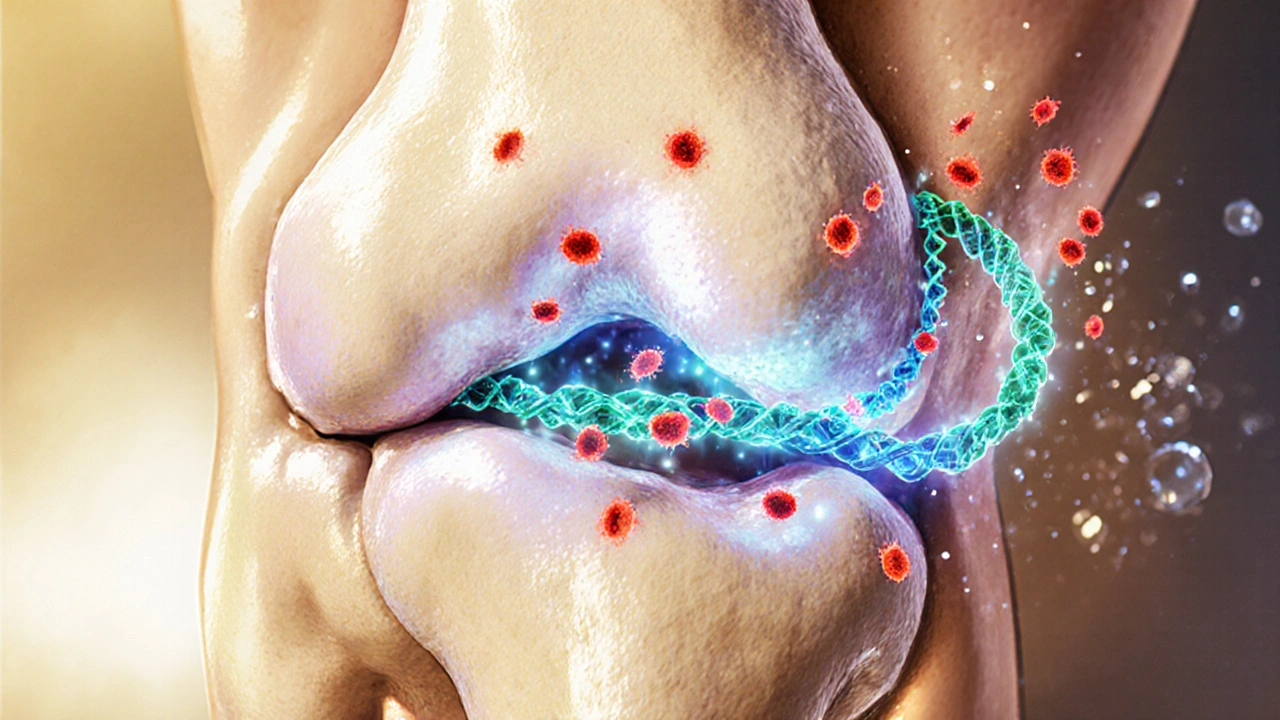
The drug belongs to a class called sulfated polysaccharides. Its backbone is a long chain of sugar residues that carries many negative charges. These charges let the molecule bind to proteins in the extracellular matrix, especially glycosaminoglycans like chondroitin and keratan sulfate. By attaching to these building blocks, pentosan polysulfate helps preserve the structural integrity of cartilage and reduces the breakdown caused by inflammatory enzymes such as interleukin‑1 and matrix metalloproteinases.
At the same time, the drug shows mild anticoagulant activity, which improves micro‑circulation around the joint. Better blood flow means nutrients reach the cartilage more efficiently, supporting repair processes.
Joint Conditions That May Benefit
- Osteoarthritis - the most common form of degenerative joint disease, primarily affecting knees, hips, and hands.
- Rheumatoid arthritis - an autoimmune condition where inflammation damages joint linings.
- Degenerative disc disease - disc cartilage loses water content, leading to pain and reduced mobility.
- Temporomandibular joint disorder (TMJ) - cartilage wear in the jaw joint can cause headaches and chewing difficulty.
- Chronic low‑back pain linked to facet joint arthritis - many patients report relief after a short course of the drug.
While the evidence base is strongest for osteoarthritis, clinicians are increasingly experimenting with the same dosing schedule for rheumatoid arthritis and disc disease, especially when patients cannot tolerate long‑term NSAIDs.
Clinical Evidence Snapshot
Three randomized, double‑blind studies published between 2018 and 2023 examined oral pentosan polysulfate in patients with knee osteoarthritis. Across the trials, the drug reduced pain scores by an average of 22 % compared with placebo and improved the WOMAC functional subscale by 18 %.
A 2022 meta‑analysis that pooled data from 7 trials (total N = 1,032) reported a statistically significant decrease in joint space narrowing after 12 months of therapy, suggesting a disease‑modifying effect rather than pure symptom relief.
For rheumatoid arthritis, a small pilot study (n = 48) showed a modest reduction in DAS28 scores after 16 weeks, but the authors cautioned that larger trials are needed to confirm the benefit.
Practical Dosing Guidelines
- Typical oral dose for joint indications is 5 mg once daily, taken with food to minimise stomach upset.
- Therapy length ranges from 6 months to a full year, depending on symptom response and radiographic monitoring.
- Blood work (CBC, PT/INR) is recommended at baseline and then every 3 months because of the drug’s mild anticoagulant effect.
- If a patient experiences a flare after stopping, a taper‑down schedule of 5 mg every other day for two weeks often avoids rebound inflammation.
Never combine pentosan polysulfate with other potent anticoagulants (e.g., warfarin, direct oral anticoagulants) without specialist advice.
Safety and Side Effects
Most users tolerate the medication well. The most common complaints are mild gastrointestinal discomfort and occasional skin rash. Rare but serious concerns include:
- Bleeding tendencies, especially in patients with clotting disorders.
- Retinal pigment epithelial changes - a visual side effect reported in a handful of long‑term users. Annual eye exams are advised for anyone on therapy beyond 12 months.
- Elevated liver enzymes in isolated cases; liver function tests should be checked at baseline.
Overall, the risk profile is more favourable than chronic NSAID use, which carries higher gastrointestinal and cardiovascular hazards.

How It Stacks Up Against Popular Supplements
| Feature | Pentosan Polysulfate | Glucosamine/Chondroitin | NSAIDs | Platelet‑Rich Plasma (PRP) |
|---|---|---|---|---|
| Primary Action | Cartilage preservation, anti‑inflammatory | Supply building blocks for cartilage | Pain relief, inflammation suppression | Growth‑factor‑driven tissue repair |
| Evidence Level | Medium - RCTs show disease‑modifying effect | Low - mixed results in meta‑analyses | High for short‑term pain control | Low‑medium - limited high‑quality trials |
| Typical Duration | 6-12 months (continuous possible) | 3-6 months (often stopped if no benefit) | As needed, usually < 2 weeks | 1‑3 injections per year |
| Side‑Effect Profile | Mild GI upset, rare bleeding, eye monitoring | Usually none, occasional GI upset | Stomach ulcer, cardiovascular risk | Injection site pain, infection risk |
| Cost (US, per month) | $150‑$250 (generic oral) | $30‑$60 | $10‑$30 (over‑the‑counter) | $500‑$1,200 (procedure) |
The table shows that pentosan polysulfate occupies a middle ground: stronger disease‑modifying data than most supplements, but a safer long‑term profile than daily NSAIDs. For patients who want to avoid steroids or surgical options, it can be a reasonable next step.
Frequently Asked Questions
Can pentosan polysulfate be used for acute joint injuries?
The drug works best on chronic, degenerative changes. For a fresh ligament tear or sprain, physiotherapy and short‑term NSAIDs remain first‑line. Some clinicians start a low dose of pentosan polysulfate once the acute inflammation subsides, hoping to speed cartilage recovery.
Is the oral form the only option?
In the United States and Europe, oral tablets are the approved formulation for joint use. An injectable version exists for bladder pain, but its dosing schedule is different and has not been studied for arthritis.
How long before I see improvement?
Most patients report noticeable pain reduction within 4‑6 weeks, while measurable changes in joint space require 6‑12 months of continuous therapy.
What should I monitor during treatment?
Baseline blood counts, coagulation profile, and liver enzymes are advisable. An annual retinal exam is recommended after the first year, especially for patients over 60.
Can I combine pentosan polysulfate with glucosamine?
There is no known interaction, and many clinicians prescribe both to cover cartilage building (glucosamine) and protection (pentosan polysulfate). Start with the lower dose and watch for any GI upset.