Imagine this: you pick up your child’s liquid antibiotics, hand the bottle to your partner, and head out the door. You don’t think twice about the number on the label-0.5 mL. But the syringe you’re given has markings in teaspoons. You measure one teaspoon, thinking it’s the same. It’s not. That one teaspoon is 5 mL-ten times the dose. Your child ends up in the hospital. This isn’t a horror story. It happened. And it happens more often than you think.
Why This One Step Saves Lives
Before you walk out of the pharmacy with your prescription, someone should be double-checking two things: the strength and the total quantity of the medication. Not just glancing. Not just assuming. Actually verifying. This isn’t just good practice-it’s a safety standard backed by decades of data and real patient harm.The Institute for Safe Medication Practices (ISMP) made this a formal best practice in 2018, and updated it in 2023. Why? Because errors in strength and quantity are among the deadliest. Insulin, opioids, blood thinners-these are high-alert medications. One wrong decimal point, one misread unit, and you’re looking at a fatal overdose. According to the FDA’s adverse event reports through mid-2023, 63% of fatal medication errors involve these kinds of mistakes.
And it’s not just about the pills. Liquid medications are the biggest culprit. A 2022 study found that 12.7% of pediatric dosing errors come from confusion over decimals-like writing 1.0 mL instead of 1 mL, or missing the leading zero (writing .5 mL instead of 0.5 mL). That’s not a typo. That’s a ten-fold overdose waiting to happen.
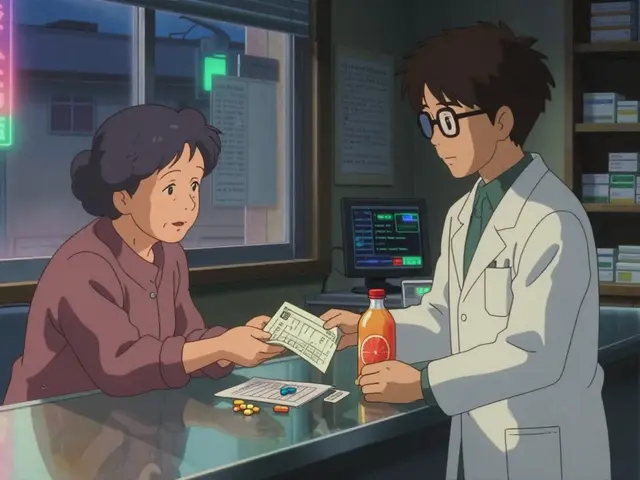
What a Real Double-Check Looks Like
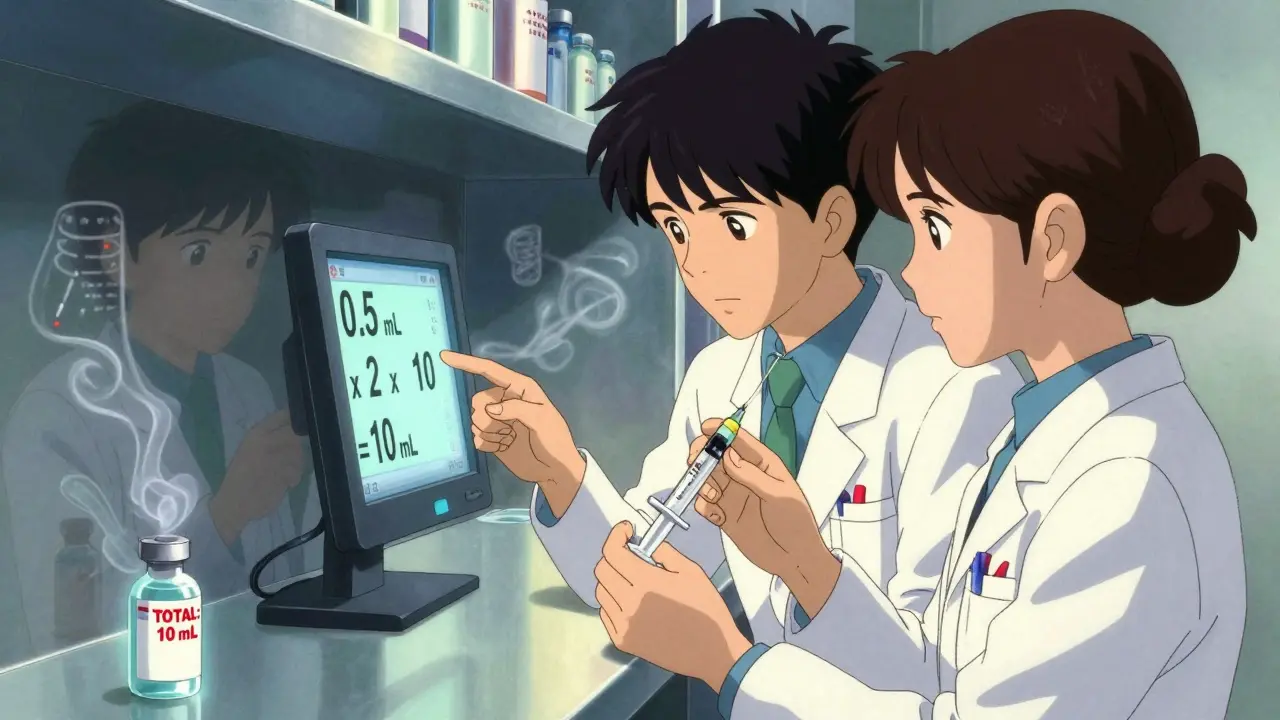
A proper double-check isn’t just one person looking at the label. It’s two people doing three things:- Confirm the strength per total volume. Is the bottle labeled as 10 mg per 5 mL? Or is it just saying 10 mg/mL? The total amount in the bottle matters. The FDA says the total drug amount must be the most prominent thing on the label-not hidden in small print. If it’s not, the pharmacy should be flagging it.
- Recalculate the total quantity. If the prescription says “take 0.5 mL twice daily for 10 days,” the total volume dispensed should be 10 mL. That’s 0.5 mL × 2 × 10. A pharmacy tech should do that math out loud, independently, and compare it to what’s in the bottle. Simple? Yes. Often skipped? Also yes.
- Match the dosing device to the prescription. Did they give you a teaspoon? That’s a red flag. The United States Pharmacopeia (USP) and NCPDP both say: use metric-only oral syringes for doses under 10 mL. Teaspoons vary. A “teaspoon” from your kitchen might hold 4 mL. Or 6 mL. An oral syringe? Exactly 0.5 mL. No guesswork.
Barcodes help. Scanning the prescription and the bottle can catch mismatches. But 83% of errors are still caught by human verification, not machines. That’s why the best pharmacies combine both: barcode scanning plus a second person recalculating the math.
What Goes Wrong When the Check Is Skipped
Pharmacists aren’t careless. But pressure is real. In community pharmacies, staff are often expected to process 35 or more prescriptions an hour. That’s less than two minutes per script. When you’re backed up, the double-check gets rushed-or skipped.On PharmacyTechForum.com, one pharmacist shared that after implementing a strict double-check system, her independent pharmacy cut strength-related errors from 1.2% to 0.15% in just one month. Three insulin errors were caught before they reached patients. That’s three lives saved.
But then there’s the Reddit post from a pharmacy tech who admitted bypassing checks during a staffing crisis. A patient got 10 times their levothyroxine dose. They ended up in the ICU. That’s not an accident. That’s a system failure.
And it’s not just about the pharmacy. The FDA found that 64% of labeling errors in drug submissions involve decimal points. A prescriber writes “0.5 mg” but the system auto-fills “5 mg.” A pharmacy receives that. If no one checks the total quantity, the patient gets the wrong dose. The chain of failure starts before the script even hits the counter.
What You Can Do as a Patient
You’re not powerless. You can-and should-be part of the safety net.- Ask: “Is this the total amount?” If you’re given a bottle of liquid medication, ask: “How much is in the whole bottle?” Compare it to what the prescription says. If the doctor ordered 10 mL total and you got 50 mL, ask why.
- Check the dosing tool. If they hand you a spoon, say no. Ask for an oral syringe. They’re free at most pharmacies. If they don’t have one, call another location. It’s worth the extra trip.
- Read the label out loud. Say it to yourself: “0.5 mL twice a day.” Does the syringe match? If the syringe says 5 mL and the label says 0.5 mL, stop. Don’t leave until it’s fixed.
- Know your meds. If you’re taking insulin, warfarin, or any high-alert drug, write down the strength and total volume. Keep it in your phone or wallet. Compare it every time you refill.
One parent told ISMP their child was hospitalized after taking 5 mL of acetaminophen instead of 0.5 mL because the pharmacy gave them a teaspoon. That child didn’t need to be in the hospital. That error was preventable.
The Bigger Picture: Why This Isn’t Just a Pharmacy Problem
This isn’t just about pharmacies being careful. It’s about a system that’s still too sloppy. The FDA’s 2023 draft guidance says that by Q3 2025, all injectable medications must have the total drug amount printed in bold, at least 50% larger than the concentration. That’s progress. But it’s still reactive.Meanwhile, Medicare Part D now requires pharmacies to prove they have strength verification protocols to stay in their network. That’s a big deal. It means insurance companies are finally holding pharmacies accountable. And the National Action Plan from AHRQ wants to cut these kinds of errors by 50% by 2027. That’s the goal.
But real change happens when patients speak up. When you ask for a syringe. When you double-check the math. When you refuse to walk out with a bottle that doesn’t make sense.
What’s Next?
The future of medication safety is digital. USP is working on a new standard called <802>, which would require electronic systems to cross-check a medication’s strength against a national database before it’s dispensed. That’s coming soon.But until then, the best defense is still a person-two people, actually-looking at the label, doing the math, and asking the right questions.
You don’t need to be a pharmacist to save a life. You just need to be awake. And you need to know: the number on the bottle isn’t always the number you’re supposed to take. Always check. Always ask. Always verify.