Alcoholism Effects Symptom Checker
Key Takeaways
- Alcoholism damages the liver, heart, brain, and immune system.
- It raises the risk of depression, anxiety, and cognitive decline.
- Physical and psychological harms reinforce each other, speeding up disease progression.
- Early warning signs include cravings, mood swings, and frequent illnesses.
- Professional help-detox, therapy, and support groups-greatly improves recovery odds.
What Is Alcoholism?
Alcoholism is a chronic disorder marked by an inability to control drinking despite adverse consequences. It’s more than just drinking a lot; the brain’s reward pathways rewire, forcing the person to seek alcohol to feel normal.
Understanding alcoholism effects helps you spot problems before they become irreversible.
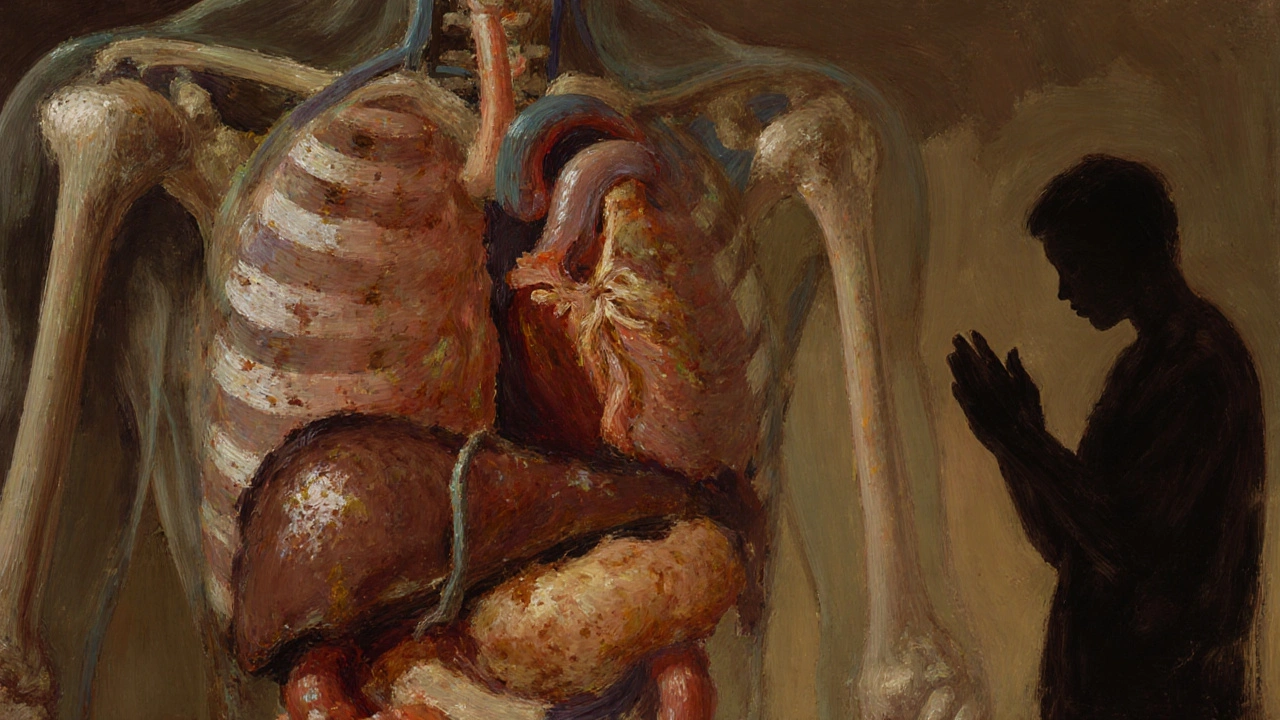
Physical Effects of Alcoholism
Heavy, long‑term drinking attacks every major organ system. Below are the most common medical problems.
- Liver disease is the most well‑known consequence, ranging from fatty liver to cirrhosis and liver cancer. The liver metabolizes alcohol, and excessive exposure creates toxic by‑products that scar tissue.
- Cardiovascular issues such as high blood pressure, irregular heartbeat, and cardiomyopathy increase the risk of stroke and heart failure.
- Pancreatitis, both acute and chronic, can cause excruciating abdominal pain and malabsorption of nutrients.
- The immune system weakens, leaving the body vulnerable to infections like pneumonia and tuberculosis.
- Alcohol‑related cancers-especially of the mouth, throat, esophagus, liver, and breast-appear at younger ages for heavy drinkers.
- Neurological damage includes peripheral neuropathy (tingling in hands/feet) and toxic encephalopathy, which can mimic dementia.
Psychological Effects of Alcoholism
The brain’s chemistry shifts dramatically under chronic alcohol exposure.
- Depression is a frequent co‑occurring mood disorder, often worsening as drinking escalates. Alcohol initially lifts mood but later depletes serotonin and dopamine.
- Anxiety is another common companion, with panic attacks and generalized worry becoming more intense during withdrawal.
- Cognitive impairment-memory lapses, reduced attention, and slowed problem‑solving-can become permanent after years of abuse.
- Sleep disturbances, including insomnia and disrupted REM cycles, increase fatigue and irritability.
- Social consequences: strained relationships, job loss, and legal troubles amplify stress and isolation.
How Physical and Psychological Effects Interact
Physical ailments often trigger or worsen mental health problems, creating a vicious cycle. For example, liver pain can fuel hopelessness, while depression may drive a person to drink more for temporary relief. This feedback loop accelerates organ damage and deepens addiction.
Short‑Term vs. Long‑Term Effects
| Aspect | Short‑Term | Long‑Term |
|---|---|---|
| Physical health | Hangover, nausea, dehydration | Organ failure, cancer, chronic diseases |
| Mental health | Impaired judgment, mood swings | Depression, anxiety, cognitive decline |
| Social life | Arguments, missed work | Relationship breakdown, legal issues |
| Risk of accidents | Increased driving crashes | Chronic injuries, motor vehicle fatalities |

Warning Signs & When to Seek Help
If you notice any of these red flags, consider professional evaluation:
- Inability to cut down despite multiple attempts.
- Drinking more than intended or hiding consumption.
- Persistent cravings and withdrawal symptoms (tremors, sweating, anxiety).
- Frequent illnesses, unexplained weight loss, or jaundice.
- Feelings of hopelessness, hopelessness, or suicidal thoughts.
Treatment Options
Recovery usually combines medical and psychosocial approaches.
- Detoxification is the medically supervised process of clearing alcohol from the body while managing withdrawal symptoms. Benzodiazepines or other medications may be used to prevent seizures.
- Behavioural therapies such as Cognitive‑Behavioural Therapy (CBT) help rewire thought patterns linked to drinking.
- Medications like naltrexone, acamprosate, or disulfiram reduce cravings or create adverse reactions to alcohol.
- Support groups are peer‑led meetings (e.g., AA) that provide accountability and shared experience. Regular attendance boosts long‑term sobriety rates.
- Holistic lifestyle changes-exercise, nutrition, sleep hygiene-support brain recovery and lower relapse risk.
Prevention and Lifestyle Tips
Even if you’re not yet dependent, these habits reduce the chance of developing alcoholism:
- Set clear drinking limits (no more than two standard drinks per day for men, one for women).
- Never drink on an empty stomach; food slows alcohol absorption.
- Find alternative stress outlets-jogging, meditation, or creative hobbies.
- Stay connected with friends and family who support a sober lifestyle.
- Seek professional help early if you notice a growing reliance on alcohol.
Frequently Asked Questions
Can occasional binge drinking cause the same health problems as chronic alcoholism?
Binge drinking spikes blood alcohol levels, which can trigger heart arrhythmias, liver inflammation, and acute brain injury. While a single episode may not cause permanent damage, repeated binges increase the risk of the same long‑term conditions seen in chronic alcoholism.
Why do some people become depressed after they stop drinking?
Alcohol artificially boosts dopamine and serotonin. When alcohol is removed, the brain’s chemistry swings low, leading to withdrawal‑induced depression. Therapy and, if needed, short‑term antidepressants help stabilize mood during recovery.
Is liver damage reversible if I quit drinking?
Early‑stage fatty liver can heal within weeks of abstinence. However, once fibrosis progresses to cirrhosis, damage is usually permanent, though stopping alcohol can prevent further decline and reduce complications.
What role does genetics play in alcoholism?
Twin and family studies show that 40‑60% of alcoholism risk is inherited. Genes affecting alcohol metabolism (e.g., ADH1B, ALDH2) and reward pathways (e.g., DRD2) influence how quickly someone becomes dependent.
How long does detox usually last?
Medical detox typically spans 5‑7days, covering the peak withdrawal window. Some people experience post‑acute withdrawal symptoms for weeks or months, which is why ongoing therapy is essential.

