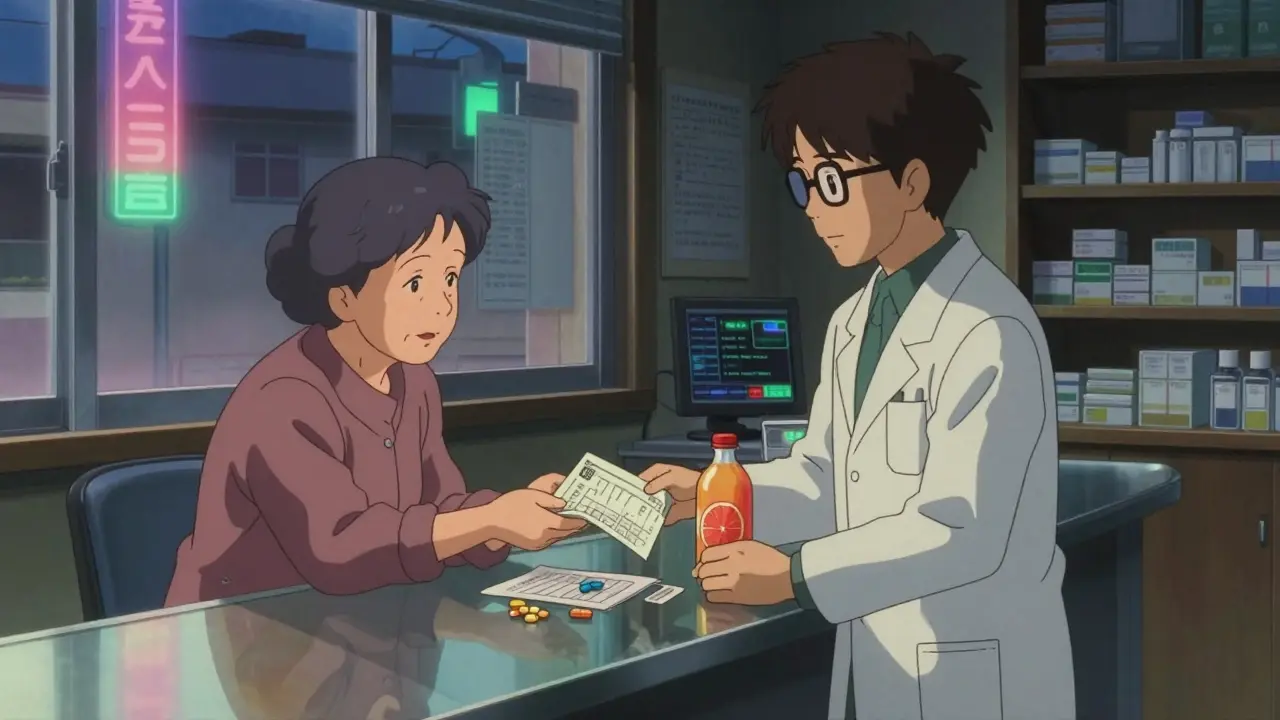
Every year, over a million people in the U.S. end up in the emergency room because of drug interactions. Many of these cases are preventable. You’re not alone if you’re taking more than one medication - or if you’re unsure whether your pills, supplements, or even your morning grapefruit juice could be working against each other. The truth is, your pharmacist is one of the most underused resources you have to stay safe. They don’t just hand out pills. They know what happens when those pills meet each other - or your food, your supplements, or your health conditions.
What exactly is a drug interaction?
A drug interaction happens when something changes how a medication works in your body. It could make it stronger, weaker, or cause unexpected side effects. There are three main types:- Drug-drug interactions: Two or more medications react. For example, taking blood thinners like warfarin with certain antibiotics can increase your risk of bleeding.
- Drug-food/beverage interactions: Some foods or drinks interfere with absorption. Grapefruit juice, for instance, can stop your body from breaking down statins, leading to dangerous muscle damage.
- Drug-condition interactions: Your existing health problem makes a drug risky. If you have high blood pressure, decongestants in cold medicines can spike your pressure to dangerous levels.
The FDA requires all prescription labels to warn about known interactions, but those warnings aren’t always clear. And they don’t cover everything - especially if you’re taking supplements or eating unusual foods.
What should you ask your pharmacist before taking a new medicine?
Don’t wait until you feel weird. Ask these questions the first time you pick up a prescription - or even before you start taking it.- Can this interact with anything else I’m already taking? Don’t just list your prescriptions. Include every over-the-counter pill, vitamin, herbal supplement, and even CBD oil. St. John’s wort, for example, can cancel out birth control pills and reduce the effectiveness of antidepressants.
- Should I avoid certain foods, drinks, or products? Grapefruit juice affects over 85 medications, including some cholesterol drugs and blood pressure pills. Alcohol can make sedatives, painkillers, and even antibiotics more dangerous. High-tyramine foods like aged cheese, cured meats, and tap beer can cause deadly blood pressure spikes if you’re on MAO inhibitors like phenelzine.
- Will this affect my existing health conditions? If you have kidney disease, liver problems, heart failure, or diabetes, some drugs can make things worse. Even something as simple as a decongestant can be risky if you have high blood pressure.
- When and how should I take this? Some meds need to be taken on an empty stomach. Others must be taken with food to reduce nausea or improve absorption. Taking them at the wrong time can reduce their effect or increase interaction risk.
- What are the warning signs I should watch for? If you start feeling dizzy, nauseous, unusually tired, or have unexplained bruising or bleeding, it could be an interaction. Ask your pharmacist what symptoms mean trouble.
- Is there a safer alternative? If your current drug has a long list of interactions, ask if another medication with fewer risks could work just as well. Sometimes switching to a different brand or class of drug makes a big difference.
Why your supplement list matters more than you think
A 2022 survey found that 77% of American adults take at least one dietary supplement. That’s a lot of hidden variables in your medication mix. Many people assume supplements are “natural” so they’re safe. That’s not true.- Vitamin K can make warfarin less effective, raising your risk of blood clots.
- Ginkgo biloba and garlic supplements can increase bleeding risk when taken with aspirin or blood thinners.
- Calcium and iron supplements can block absorption of thyroid meds like levothyroxine if taken at the same time.
Pharmacists see this all the time. One patient took a daily multivitamin with iron and noticed their blood pressure medicine wasn’t working. Turns out, the iron was blocking absorption. Once they spaced them out by four hours, their numbers improved.

How to prepare for your pharmacist visit
Don’t show up with a vague memory of what you take. Bring this:- A printed or digital list of every medication - including name, dose, and how often you take it.
- All your supplements, vitamins, and herbal products in their original bottles (or photos of the labels).
- Your most recent lab results if you’re on chronic meds (like kidney or liver function tests).
- A note about your diet: Do you drink grapefruit juice daily? Do you drink alcohol? Do you eat a lot of leafy greens or aged cheeses?
Pharmacists use this info to run real-time checks against databases that flag over 100,000 possible interactions. But they can’t help if they don’t have the full picture.
What pharmacies are doing to help - and where they still fall short
Most big pharmacy chains now use digital systems that scan your profile for interactions when you pick up a prescription. But a 2022 study in JAMA Internal Medicine found these systems miss nearly 1 in 5 dangerous interactions. Why? Because they rely on what’s in your file - and many patients don’t tell pharmacists about every supplement, or forget to update them when they stop or start something.That’s why your role matters. Even if the system flags nothing, ask anyway. Pharmacists are trained to look beyond the screen. They know that a 72-year-old woman on five medications might be at higher risk than the algorithm suggests.

When to talk to your pharmacist - not just when you pick up a script
Don’t wait for your next refill. Talk to your pharmacist whenever:- You start a new medication - even if it’s over-the-counter.
- You stop taking something.
- You change your dose.
- You get a new diagnosis (like diabetes or kidney disease).
- You start or stop using alcohol, tobacco, or herbal products.
According to experts at Cedars-Sinai, the most common cause of a new interaction is the most recent drug added. So every new pill - even a pain reliever - should trigger a quick check.
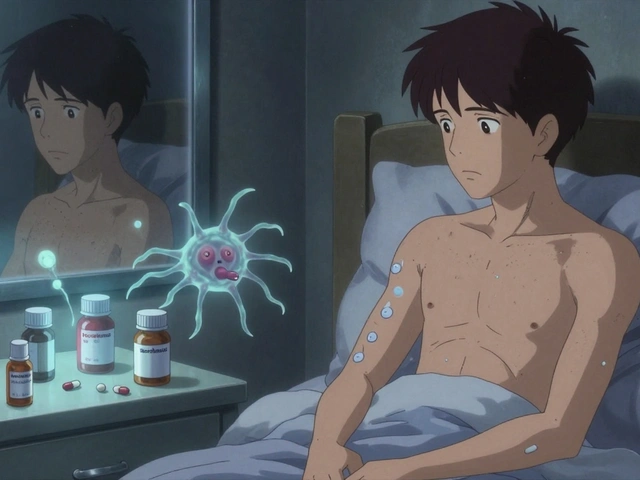
What happens if you don’t ask?
The risks aren’t theoretical. In 2022, over 112,000 adverse events linked to drug interactions were reported to the FDA. The most common culprits? Blood thinners, diabetes meds, and heart drugs. These aren’t rare cases. They’re preventable.One man in his 60s took a common cholesterol drug and started having muscle pain. He didn’t think it was serious - until he collapsed. Turns out, he was also taking a common antibiotic that blocked how his body processed the statin. His blood levels spiked. He needed hospitalization. He didn’t know to ask about the interaction.
Another woman took melatonin for sleep and started having weird bruising. Her pharmacist found she was also on a blood thinner. Melatonin can thin the blood further. A simple conversation prevented a major bleed.
These stories aren’t outliers. They’re routine.
Final tip: Make it a habit
Set a reminder every three months to review your meds with your pharmacist. Even if nothing changed, it’s worth a quick check. Your body changes. Your meds change. Your habits change. So should your safety plan.Pharmacists aren’t just there to fill prescriptions. They’re your medication safety net. And the more you ask, the better they can protect you.
What should I do if I think I’m having a drug interaction?
Stop taking the medication immediately and call your pharmacist or doctor. Don’t wait to see if symptoms go away. Write down what you took, when, and what symptoms you’re feeling. If it’s an emergency - like chest pain, trouble breathing, or severe bleeding - go to the nearest emergency room. Bring your medication list with you.
Can I trust online interaction checkers?
Online tools can be helpful for a quick check, but they’re not foolproof. Many don’t include supplements, herbal products, or dietary habits. They also don’t know your medical history or how your body processes drugs. Always confirm results with your pharmacist. They have access to clinical databases and can interpret your personal risk.
Do I need to tell my pharmacist about vitamins and supplements?
Yes - absolutely. Supplements aren’t regulated like prescription drugs, so their ingredients and strengths can vary. Many have active compounds that interact with medications. For example, vitamin E and fish oil can increase bleeding risk with blood thinners. Even common ones like calcium or magnesium can interfere with thyroid or antibiotic absorption. Your pharmacist needs the full list to keep you safe.
Why does grapefruit juice interact with so many drugs?
Grapefruit juice blocks an enzyme in your gut called CYP3A4, which normally breaks down certain drugs. When that enzyme is blocked, the drug builds up in your bloodstream - sometimes to toxic levels. This affects statins, some blood pressure meds, anti-anxiety drugs, and others. Even one glass can cause an interaction that lasts over 24 hours. If you’re on any medication, ask if grapefruit is safe - and if so, how much.
Can my pharmacist change my prescription?
No, only your doctor can change your prescription. But your pharmacist can suggest alternatives, flag risks, and communicate with your doctor on your behalf. Many pharmacists now have collaborative practice agreements that let them adjust doses or switch meds under certain conditions - especially in chronic disease management. Ask if your pharmacy offers this service.
How often should I get my meds reviewed?
At least once a year - but ideally every three months if you take five or more medications. If you’ve had a new diagnosis, started or stopped a drug, or changed your diet or lifestyle, schedule a review right away. The more meds you take, the higher the risk of interactions. Regular reviews are not optional - they’re essential.
What if I can’t afford to see a pharmacist?
Most pharmacies offer free medication reviews with every prescription pickup. You don’t need an appointment. Just ask: “Can you check if these meds interact?” Many also offer free counseling sessions for patients on multiple drugs. If you’re on Medicare, you’re eligible for Medication Therapy Management (MTM) services at no extra cost. Don’t assume it’s expensive - it’s often free.