Warfarin Antibiotic INR Calculator
Calculate Your INR Risk
Estimate how your current INR might change when taking common antibiotics.
When you’re on warfarin, even a simple antibiotic can throw your blood thinning off balance-sometimes dangerously. It’s not just about taking pills. It’s about understanding how your body reacts when two common medications collide. For someone managing atrial fibrillation, a mechanical heart valve, or deep vein thrombosis, an unexpected rise in INR isn’t just a lab number. It’s a red flag for internal bleeding. And antibiotics? They’re one of the most common triggers.
Why Antibiotics Change Your INR
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. But your gut bacteria also make vitamin K-about 10-15% of what you need. When you take certain antibiotics, you kill off those helpful bacteria. That means less vitamin K, more warfarin effect, and a rising INR. This doesn’t happen right away. It usually takes 5 to 7 days after starting the antibiotic.There’s another, faster way antibiotics interfere: liver enzymes. Warfarin is broken down mostly by CYP2C9, a liver enzyme. Some antibiotics block this enzyme, causing warfarin to build up in your blood. This spike can happen in just 48 to 72 hours. The result? INR climbs. And when INR goes above 4.0, your risk of major bleeding jumps 4 to 8 times.
Which Antibiotics Are Most Dangerous?
Not all antibiotics are equal when it comes to warfarin. Some are low-risk. Others are ticking time bombs.- High risk: Ciprofloxacin, levofloxacin (fluoroquinolones), erythromycin, sulfamethoxazole/trimethoprim (Bactrim), and amoxicillin/clavulanate. These can raise INR by 1.5 to 2.5 units on average. Ciprofloxacin alone has been linked to INR spikes from 2.5 to 4.1 in just a week.
- Medium risk: Cefotetan and cefoperazone (cephalosporins with NMTT side chains). They don’t affect liver enzymes but wipe out gut bacteria. INR can rise by 1.5 to 2.2 units.
- Low risk: Azithromycin, ceftriaxone, nitrofurantoin, and fosfomycin. These rarely cause INR changes. Azithromycin, for example, increases bleeding risk by only 1.2 times compared to 2.3 times with erythromycin.
- Opposite effect: Rifampin. This one speeds up warfarin breakdown. Instead of INR rising, it crashes-sometimes below 1.5. That means clots, not bleeding. You’ll need a higher warfarin dose, not lower.
Here’s what the data says: A 2018 meta-analysis found ciprofloxacin increases bleeding risk by 2.1 times. Bactrim? 1.8-unit INR rise in five days. Amoxicillin/clavulanate? Average INR increase of 1.2 units. And rifampin? Can cut warfarin levels by 60%. You can’t guess. You have to test.
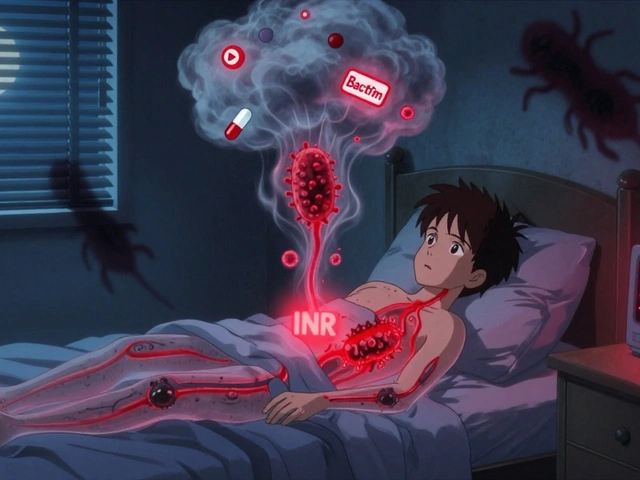
When to Check Your INR
The American College of Chest Physicians says this clearly: Check your INR within 72 hours of starting any antibiotic. Then check again weekly until the antibiotic ends-and for a few days after.Why? Because the danger doesn’t disappear when you stop the antibiotic. Gut bacteria take time to recover. INR can keep climbing for another week after the last pill. Studies show bleeding risk peaks between days 8 and 14 of antibiotic use. That’s after you think you’re safe.
For high-risk antibiotics like ciprofloxacin or Bactrim, check INR every 2-3 days. For medium-risk ones like amoxicillin/clavulanate, weekly is usually enough-unless your INR starts to climb. And if you’re on rifampin? Daily INR checks for the first week. Your dose will likely need to go up by 50% or more.

What to Do When INR Rises
If your INR is too high but you’re not bleeding:- For INR 4.0-5.0: Skip your next 1-2 warfarin doses. Recheck INR in 2-3 days.
- For INR 5.0-9.0: Skip doses and take 1-2 mg of oral vitamin K. Recheck in 24-48 hours.
- For INR >9.0 or active bleeding: Go to the ER. You’ll likely need IV vitamin K and possibly fresh frozen plasma.
Never adjust your dose on your own without talking to your anticoagulation clinic. A 20%-30% warfarin dose reduction at the start of high-risk antibiotics can prevent spikes-but only if done under supervision. One study found that patients who had their dose lowered preemptively had 4.7 times less major bleeding than those who didn’t.
What You Can Do at Home
You’re not just a patient-you’re part of the safety team.- Know the signs of bleeding: Unexplained bruising, blood in urine or stool, nosebleeds that won’t stop, severe headaches, dizziness, or pain in joints or abdomen.
- Keep a log: Write down every antibiotic you take, the date you started, and your INR results. Bring it to every appointment.
- Ask your pharmacist: Before filling any new prescription, ask, “Will this interact with my warfarin?” Pharmacists who manage warfarin therapy reduce bleeding by 37% compared to doctor-only care.
- Don’t skip appointments: Even if you feel fine, INR changes can be silent.
Some people think, “I’ve taken amoxicillin before with no problem.” But your gut bacteria change. Your liver enzymes change. Your warfarin sensitivity changes. Yesterday’s safe dose isn’t today’s safe dose.
What’s New in 2025
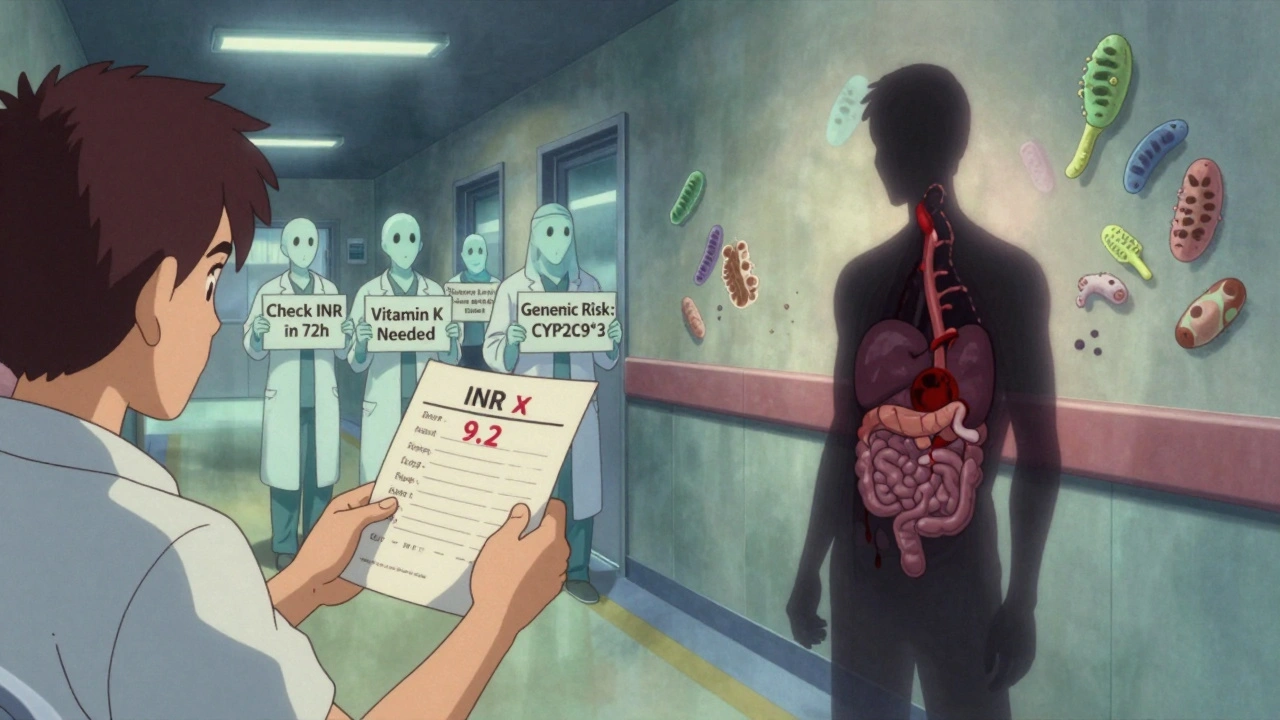
The field is moving fast. In 2024, researchers confirmed that even cephalosporins like cefotetan carry a 1.9-fold higher bleeding risk than previously thought. New antibiotics like tedizolid are now known to be safe-no INR changes expected.Genetic testing is becoming more common. If you have the CYP2C9*2 or *3 gene variant, your body breaks down warfarin slower. When you add an antibiotic, your INR can spike 2.4 times higher than someone without the variant. The 2023 WARF-GEN trial showed that testing for these genes before starting antibiotics cut INR instability by 41%.
Electronic alerts in hospitals help-but only if they’re paired with real clinical advice. Alerts alone reduced bad events by just 7%. With pharmacist follow-up, it jumped to 22%.
Bottom Line: Stay Alert, Stay Informed
Antibiotics and warfarin don’t mix blindly. Every antibiotic has a different effect. Every person has a different risk. There’s no one-size-fits-all answer.What you need is vigilance: Know which antibiotics are risky. Check your INR at the right times. Listen to your body. Talk to your care team. Don’t assume safety because you’ve done it before. The next time you’re prescribed an antibiotic, ask: “Could this raise my INR?” That one question might save your life.