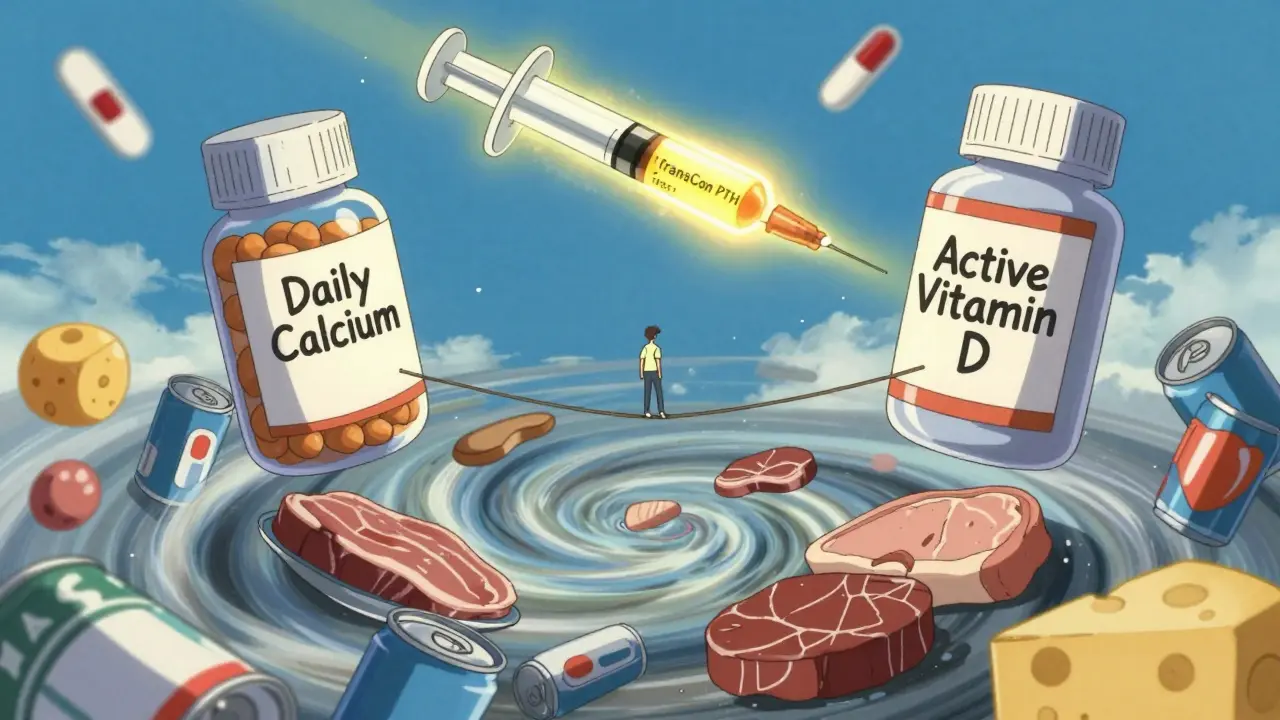
When your parathyroid glands don’t make enough hormone, your body can’t keep calcium in balance. That’s hypoparathyroidism - a rare but serious endocrine disorder that leaves you with low calcium, high phosphate, and symptoms that can sneak up on you: tingling fingers, muscle cramps, fatigue, or even seizures if left untreated. Most people get it after thyroid or neck surgery, but it can also come from autoimmune issues or genetics. The good news? You can manage it. The challenge? It’s not simple. You’re not just taking a pill and calling it done. You’re managing a tightrope walk between too little calcium and too much in your kidneys.
Why Calcium and Vitamin D Are Non-Negotiable
Parathyroid hormone (PTH) normally tells your bones to release calcium, your kidneys to hold onto it, and your gut to absorb more from food. Without it, calcium drops fast. That’s why treatment isn’t about fixing PTH - it’s about replacing what it does. Calcium and active vitamin D become your body’s substitute crew.
Here’s the catch: regular vitamin D (cholecalciferol) won’t cut it. Your kidneys need PTH to turn it into the active form. So doctors prescribe calcitriol or alfacalcidol - already activated versions that skip that broken step. Studies show these work 2.3 times faster than regular vitamin D at raising calcium levels. You’ll typically start with 0.25 to 0.5 micrograms daily, adjusted based on blood tests.
Calcium supplements are your other main tool. Calcium carbonate is preferred because it packs more elemental calcium - 40% - than citrate (only 21%). That means you need fewer pills. Most people start with 1,000 to 2,000 mg of elemental calcium per day, split into two or three doses taken with meals. Why with food? It helps absorption and also acts as a phosphate binder, which is key because phosphate levels tend to climb when PTH is low.
The Target: Stable, Not Perfect
There’s no magic number. But experts agree: aim for the lower half of normal. That’s 2.00 to 2.25 mmol/L (or 8.0 to 8.5 mg/dL). Pushing higher might stop your tingling, but it risks calcium building up in your kidneys, brain, or blood vessels. One study found patients with levels above 2.35 mmol/L had nearly three times the risk of brain calcification after 15 years.
That’s why frequent blood tests matter. In the first few months, you’ll likely need them every 1 to 3 months. Once stable, you can cut back to every 4 to 6 months. But don’t forget the urine test. A 24-hour urinary calcium check is critical. If you’re excreting more than 250 mg per day, you’re on track for kidney stones or damage. This isn’t optional - it’s the safety net.
What If Your Numbers Won’t Cooperate?
One in four people with hypoparathyroidism struggles to get stable, even with high doses. If you’re taking more than 2 grams of calcium or 2 micrograms of active vitamin D daily and still having symptoms, you’re in the tough group. This is where things get complicated.
First, check your magnesium. Low magnesium (below 1.7 mg/dL) makes calcium and vitamin D work poorly - even if your levels look fine. You might need 400 to 800 mg of magnesium oxide daily. Many patients don’t know this until they’re stuck in a cycle of worsening symptoms.
Second, look at your diet. Phosphate is the silent saboteur. Soda, processed meats, hard cheeses, and even some breads are loaded with it. Cutting back to 800-1,000 mg per day helps. Swap soda for water. Choose fresh chicken over deli meat. Eat broccoli instead of cheese on your salad. These aren’t suggestions - they’re part of the treatment.
Third, if you’re still struggling, thiazide diuretics like hydrochlorothiazide (12.5-25 mg daily) can help your kidneys hold onto calcium instead of flushing it out. This is a common trick for patients with persistent high urinary calcium.
The New Hope: PTH Replacement
For those who can’t get control with pills, there’s a newer option: actual PTH replacement. Natpara (recombinant human PTH 1-84) and Forteo (teriparatide) are injectables that mimic the real hormone. They don’t just raise calcium - they reduce your need for calcium pills and vitamin D by 30-40%. In one trial, patients on PTH replacement had fewer kidney problems and better bone health.
But it’s not easy. Natpara costs about $15,000 a month. Insurance fights it. You need a specialty pharmacy. Prior authorization can take 30 to 45 days. You have to inject it daily. And it comes with a black box warning for bone cancer risk in rats - though no human cases have been confirmed.
Still, for someone taking 10 pills a day, dealing with constant fatigue, and terrified of kidney stones, it’s life-changing. A 2022 trial of a new long-acting PTH drug called TransCon PTH showed 89% of patients reached normal calcium levels with just one weekly injection. That’s the future - and it’s coming faster than most realize.
Living with the Rollercoaster
Patients describe it as a “calcium rollercoaster.” One day you’re fine. The next, your hands cramp, your face feels numb, your heart races. Why? Timing. Calcium doesn’t stay in your blood for long. Taking big doses twice a day leads to spikes and crashes.
Try splitting it: four or five smaller doses spread through the day. Take one with breakfast, one with lunch, one with dinner, and one before bed. Parathyroid UK recommends this for better stability. Many patients report fewer symptoms and less anxiety.
Also, never skip meals. Calcium taken without food doesn’t absorb well. And if you’re sick, stressed, or traveling - your needs change. Always carry emergency calcium tablets. Chewing two or three (500-1,000 mg elemental calcium) can stop a full-blown crisis before it hits the ER.
What Your Doctor Might Not Tell You
Most family doctors haven’t managed a hypoparathyroidism case in years. A 2021 survey found 78% of them felt unprepared. That’s why you need an endocrinologist - at least initially. You need someone who knows to check urinary calcium, who understands the difference between calcitriol and cholecalciferol, and who won’t just up your dose when you’re symptomatic.
And don’t ignore mental health. One in two patients reports daily symptoms despite treatment. The constant checking of blood levels, the pill burden, the fear of a seizure - it wears you down. Support groups like the Hypopara Alliance (with over 400 members) aren’t just helpful. They’re essential.
Long-Term Risks You Can’t Ignore
People live with this for decades. But long-term conventional therapy isn’t harmless. About 15-20% develop chronic kidney disease after 10 years. Calcium deposits can form in your brain, eyes, or heart valves. The goal isn’t just to feel okay today - it’s to protect your body for tomorrow.
That’s why the new guidelines stress caution. Don’t chase normal calcium. Chase stable, low-normal. Avoid high-dose calcium unless absolutely necessary. Monitor urine. Watch your diet. Test magnesium. And always ask: is this helping me now - or hurting me later?
What You Can Do Today
- Start with calcium carbonate - 1,000-2,000 mg elemental calcium daily, split into 3-4 doses with meals.
- Take calcitriol or alfacalcidol as prescribed - not regular vitamin D.
- Get a 24-hour urine calcium test - and repeat it before any dose increase.
- Check your magnesium. If it’s below 1.7 mg/dL, start supplementing.
- Cut out soda, processed meats, and hard cheeses. Choose fresh food.
- Carry calcium tablets with you at all times.
- Find an endocrinologist who knows this condition - don’t settle for general advice.
Hypoparathyroidism isn’t curable - yet. But it’s manageable. With the right balance of medicine, diet, and monitoring, you can live well. It’s not about perfection. It’s about consistency. And knowing when to push back - on your doctor, on your insurance, on your own limits - is just as important as the pills you take.

