Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) aren’t just rare skin conditions-they’re life-threatening emergencies that can start with a simple headache or sore throat. What begins as something mild can spiral into a full-body crisis within days. If you or someone you know has recently started a new medication and suddenly develops a painful rash, blisters, or sores in the mouth or eyes, this isn’t something to wait out. Stevens-Johnson Syndrome and TEN are extreme reactions to drugs, and they demand immediate medical care.
How SJS and TEN Are Connected
For years, doctors thought SJS and TEN were two different diseases. Now we know they’re part of the same spectrum-one continuum of severe skin damage. The difference comes down to how much of your skin is affected. If less than 10% of your body surface area (BSA) is peeling off, it’s classified as SJS. If it’s between 10% and 30%, it’s called overlap syndrome. But if more than 30% of your skin detaches, that’s TEN-the most dangerous form.
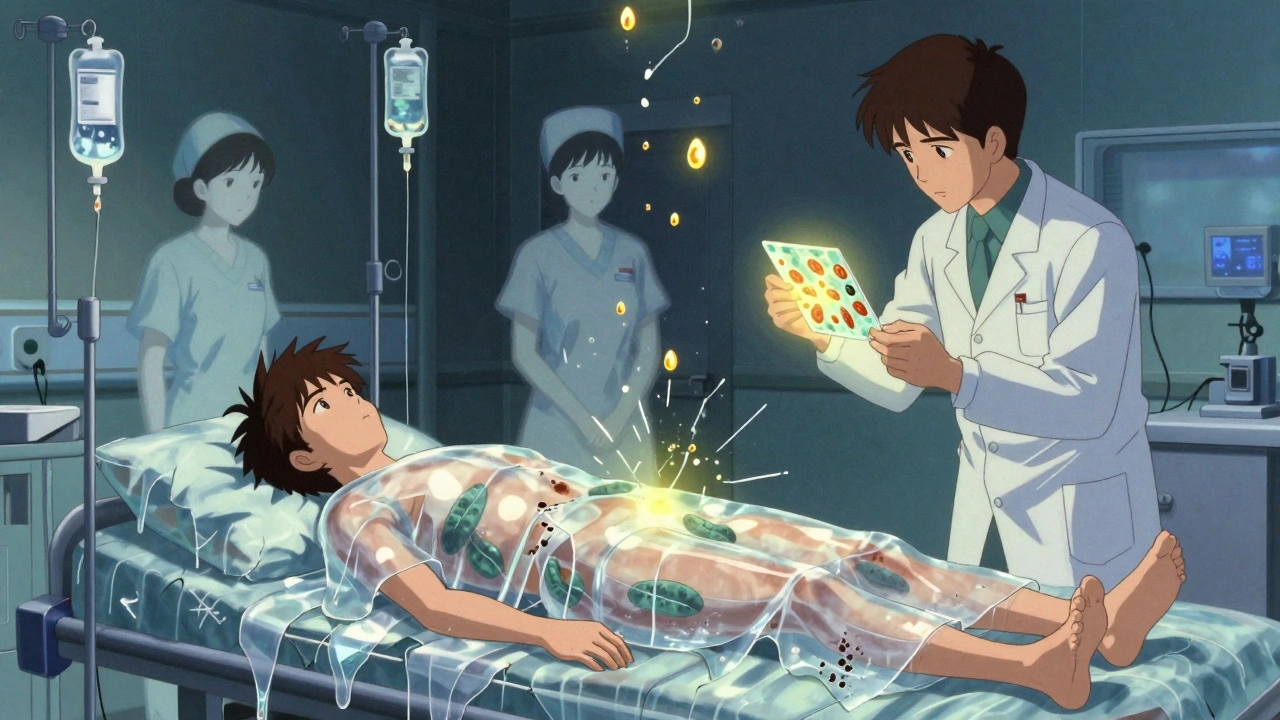
Think of it like a burn. In TEN, large sheets of skin slough off, leaving raw, wet, painful areas that look like third-degree burns. The skin doesn’t just blister-it literally separates from the body. This isn’t a rash you can treat with cream. It’s a systemic collapse of the skin barrier, and it happens fast.
What Triggers These Reactions?
Over 80% of cases are caused by medications. The most common culprits are specific drugs that millions of people take every day:
- Antiepileptics: carbamazepine, phenytoin, lamotrigine
- Sulfonamide antibiotics: like trimethoprim-sulfamethoxazole (Bactrim)
- Allopurinol: used for gout
- NSAIDs: especially when taken long-term or at high doses
- Nevirapine: an HIV medication
It’s not about how much you take-it’s about your genetics. Certain people carry a gene variant called HLA-B*15:02. If you have this gene and take carbamazepine, your risk of SJS/TEN jumps by up to 1,000 times. For allopurinol, the HLA-B*58:01 gene raises risk by 80 to 580 times. That’s why countries like Taiwan now require genetic testing before prescribing these drugs. In the U.S., the FDA now recommends screening for high-risk groups before starting treatment.
Less than 10% of cases are triggered by infections-most commonly Mycoplasma pneumoniae, especially in children. But even then, the reaction looks identical to the drug-induced kind. That’s why doctors treat them the same way: stop everything, get to the hospital, and act fast.
What Happens When It Starts?
The warning signs come before the skin breaks down. You might feel like you’re coming down with the flu: fever above 38.9°C (102°F), sore throat, cough, burning eyes, or general fatigue. This phase lasts one to three days. Then, the skin changes.
Red or purple spots appear-usually on the chest, back, or face. They’re flat at first, not raised. Within 24 to 72 hours, they turn into blisters that merge into large, loose sheets of skin. The blisters rupture easily. When you press on the skin near a blister, the surrounding area peels off-that’s called the Nikolsky sign, and it’s a red flag for SJS/TEN.
Mucous membranes are always involved. You’ll likely have painful sores in your mouth (90% of cases), eyes (80%), genitals (60%), and sometimes your throat or lungs. Eating, drinking, or even opening your eyes becomes unbearable. Many patients describe it as being burned alive from the inside out.
Why Is It So Dangerous?
When skin detaches, your body loses its protection. Fluids leak out. Heat escapes. Bacteria rush in. This is why people with TEN are treated like burn victims-in specialized burn units, not regular wards. Your body can lose liters of fluid a day. Blood pressure drops. Kidneys struggle. Infections set in fast. Sepsis is the leading cause of death.
The SCORTEN scale helps doctors predict survival. It looks at seven factors within the first 24 hours: age over 40, cancer history, heart rate over 120, more than 10% skin detachment, high blood sugar, high urea levels, and low bicarbonate. Each factor increases your risk. Three factors mean a 35% chance of dying. Five or more? The risk jumps to 90%.
How Is It Diagnosed?
There’s no single blood test. Diagnosis relies on three things: your symptoms, your medication history, and a skin biopsy. The biopsy shows full-thickness skin death-keratinocytes dying en masse-with almost no inflammation in the deeper layers. That’s what sets it apart from other blistering diseases like staphylococcal scalded skin syndrome, which affects kids and has different under-the-skin damage.
Doctors also rule out other conditions like pemphigus or drug-induced pustular rashes. Misdiagnosis can be deadly. If you’re told it’s just a viral rash and sent home, you could die within 48 hours.
What’s the Treatment?
Step one: stop every non-essential medication. That includes vitamins, supplements, over-the-counter painkillers. Even if you think it’s safe, everything gets paused until the cause is clear.
Step two: intensive care. You need fluids-three to four times what a healthy person needs. You need sterile, non-stick dressings. You need pain control that actually works. You need daily eye exams to prevent blindness from scarring. You need nutrition support because your mouth is too sore to eat.
There’s debate over what drugs help. IVIG (intravenous immunoglobulin) was once widely used, but large studies now show it doesn’t improve survival. Steroids are risky-they increase infection chances-but some doctors use high-dose pulses early on. Cyclosporine, an immune suppressant, showed better survival in a 2016 trial: mortality dropped from 33% to 12.5%.
The most promising new treatment is etanercept, a drug that blocks tumor necrosis factor (TNF-alpha). In a 2019 study, 12 patients with TEN who got etanercept within 48 hours had zero deaths. The historical death rate for similar cases was over 30%. That’s a game-changer.
What Happens After You Survive?
Surviving SJS/TEN doesn’t mean you’re back to normal. Sixty to eighty percent of survivors face long-term problems:
- Chronic dry eyes, light sensitivity, corneal scarring (50-80%)
- Permanent skin discoloration (70%) or scarring (40%)
- Nail loss or deformed nails (25%)
- Urethral narrowing or vaginal scarring (10-15%)
- Post-traumatic stress disorder (PTSD) in 40% of survivors
Many people need years of follow-up: ophthalmologists, dermatologists, gynecologists, psychologists. Some require reconstructive surgery. The trauma of being hospitalized for weeks, unable to speak or open your eyes, leaves deep psychological scars.

Can It Be Prevented?
Yes-and it’s happening already. In places with mandatory HLA screening before prescribing high-risk drugs, SJS/TEN cases have dropped by 80%. Taiwan’s program, started in 2007, saved hundreds of lives. The FDA approved a point-of-care HLA-B*58:01 test in 2022-results in four hours instead of two weeks.
If you’re prescribed carbamazepine, lamotrigine, allopurinol, or sulfonamides, ask: “Have you checked my HLA genes?” If you’re Asian, especially of Han Chinese, Thai, or Malaysian descent, this screening is critical. Even if you’re not, if you’ve had a severe rash from a drug before, tell your doctor.
There’s no cure for SJS/TEN-but we now have the tools to prevent most cases. And if it happens, faster diagnosis and targeted treatments like etanercept are turning a death sentence into a survivable emergency.
What Should You Do If You Suspect It?
If you or someone you know develops:
- A sudden fever and sore throat after starting a new drug
- Painful red or purple spots on the skin
- Blisters or peeling skin
- Sores in the mouth, eyes, or genitals
-go to the emergency room immediately. Don’t wait. Don’t call your GP. Don’t try home remedies. This is a medical emergency. Bring a list of all medications you’ve taken in the last four weeks, including supplements and over-the-counter drugs.
Can Stevens-Johnson Syndrome be caused by vaccines?
There’s no strong evidence linking vaccines to SJS or TEN. Less than 1% of cases are tied to vaccines, and most of those are anecdotal or poorly documented. The overwhelming majority of cases-over 80%-are caused by prescription medications like antiepileptics, antibiotics, or allopurinol. If you’re concerned about a vaccine reaction, talk to your doctor, but don’t avoid vaccines based on fear of SJS/TEN.
Is Stevens-Johnson Syndrome contagious?
No, SJS and TEN are not contagious. You can’t catch it from someone else. It’s an immune reaction triggered by your own body’s response to a drug or infection. You can safely care for someone with SJS/TEN without risk of infection-though you should follow hospital hygiene rules to protect their vulnerable skin.
Can you get SJS/TEN more than once?
Yes, but only if you’re re-exposed to the same drug or a closely related one. If you’ve had SJS/TEN from carbamazepine, you must avoid carbamazepine and all similar antiepileptics for life. Cross-reactivity is common-so if one drug caused it, others in the same class likely will too. Genetic testing helps identify which drugs to avoid permanently.
How long does recovery take?
Skin regeneration takes 2-4 weeks, but full recovery can take months to years. The initial hospital stay averages 2-6 weeks. Long-term issues like dry eyes, scarring, and psychological trauma can last a lifetime. Many survivors need ongoing care from multiple specialists. Recovery isn’t just physical-it’s emotional and social, too.
Are children at risk for SJS/TEN?
Children can get SJS/TEN, but it’s rarer than in adults. Infections like Mycoplasma pneumoniae are more common triggers in kids. The same high-risk drugs can still cause it, but genetic testing isn’t routinely done in children unless there’s a family history or prior reaction. Parents should watch for sudden fever, mouth sores, or rash after starting antibiotics or fever reducers.
Final Thoughts
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis are terrifying, but they’re not inevitable. We now understand the triggers, the genetic risks, and the treatments that save lives. The key is awareness. If you’re on a high-risk medication, know the signs. If you’ve had a bad reaction before, tell every doctor you see. And if something feels wrong-don’t ignore it. Early action can mean the difference between life and death.

