When a patient walks into the pharmacy with a prescription for a brand-name drug, the pharmacist’s first thought shouldn’t just be about cost-it should be about authorized generics. These aren’t your typical generic pills. They’re the exact same medication as the brand, made by the same company, with the same active and inactive ingredients, just sold without the brand name on the label. And in certain cases, they’re the safest, smartest choice.
What Exactly Is an Authorized Generic?
An authorized generic is not a copy. It’s the original drug-same formula, same manufacturer, same quality control-just repackaged under a different name. The FDA defines it clearly: it’s a brand-name drug approved under a New Drug Application (NDA) that’s sold without the brand’s trademark, logo, or packaging. The pill inside? Identical. The fillers? The same. The coating? Unchanged.
This isn’t the same as a regular generic. Regular generics must prove they’re bioequivalent to the brand through testing. Authorized generics skip that step because they’re the exact same product. They’re made on the same生产线, in the same factory, by the same team that makes the brand. The only difference? The label says “Lisinopril 10 mg” instead of “Zestril.”
The FDA has been tracking these since 1999. As of September 2023, there were 257 authorized generics on the market-about 5% of all brand-name drugs with generic alternatives. Most are oral tablets or capsules. And they’re not rare outliers-they’re strategic tools used by manufacturers to compete with generic entrants.
When Pharmacists Should Recommend Authorized Generics
Not every patient needs an authorized generic. But for some, it’s the only safe option.
1. Patients With Allergies or Dietary Restrictions
Regular generics often use different inactive ingredients-fillers, dyes, preservatives-than the brand. That’s fine for most people. But for someone with celiac disease, gluten in the filler can trigger serious reactions. For someone avoiding animal products, gelatin capsules or lactose binders can be a dealbreaker.
Authorized generics avoid this problem. Since they use the exact same inactive ingredients as the brand, they’re safe for patients who’ve already tolerated the brand. A patient who had no issues with brand-name Levoxyl? An authorized generic version of levothyroxine is the only safe generic substitute. Regular generics might have different fillers that could cause a reaction-even if the active ingredient is identical.
2. Narrow Therapeutic Index (NTI) Drugs
Some medications have a razor-thin margin between effective and toxic doses. Warfarin, phenytoin, levothyroxine, and lithium fall into this category. A tiny change in absorption can mean the difference between control and crisis.
Studies show that 3-5% of patients on NTI drugs experience problems after switching from brand to regular generic-even when the generic is labeled “therapeutically equivalent” in the Orange Book. Why? Because bioequivalence testing doesn’t capture subtle differences in how the drug is released or absorbed over time.
Authorized generics eliminate that risk. No formulation changes. No new excipients. No uncertainty. For patients on warfarin, switching to an authorized generic means less need for frequent INR checks and fewer hospital visits.
3. Modified-Release Formulations
Drugs like extended-release metformin, controlled-release oxycodone, or delayed-release omeprazole rely on complex delivery systems. Regular generics may use different polymers or coatings to mimic the release profile, but they don’t always perform the same way in real-world use.
Patients on these drugs often report unexpected side effects or reduced effectiveness after switching. A 2021 survey of 1,200 community pharmacists found that 12% of patients experienced problems after switching to a regular generic. In these cases, the authorized generic is the most reliable alternative-it’s the original delivery system, just without the brand name.
4. When Patients Report Unexpected Side Effects
If a patient says, “I’ve been taking this for years, but since I switched to the generic, I’ve had headaches and nausea,” don’t assume it’s psychosomatic. It could be the filler. The dye. The coating.
Before jumping to a new brand or calling the prescriber, check if an authorized generic exists. It’s often the missing piece. Many patients don’t realize the pill changed-just that they feel different. A simple switch to an authorized generic can restore stability without changing the prescription.
How to Spot an Authorized Generic
They don’t show up in the Orange Book. You won’t find them listed as “AB-rated.” That’s because they’re not separate products-they’re the brand in disguise.
To identify one, check the National Drug Code (NDC). Look at the labeler code. If it matches the brand manufacturer (Pfizer, Merck, AbbVie) or an authorized licensee like Prasco or Greenstone, it’s an authorized generic. If it’s a company like Teva, Mylan, or Sandoz, it’s a regular generic.
The FDA updates its list of authorized generics quarterly. Bookmark it. Use it. It’s the only official source.
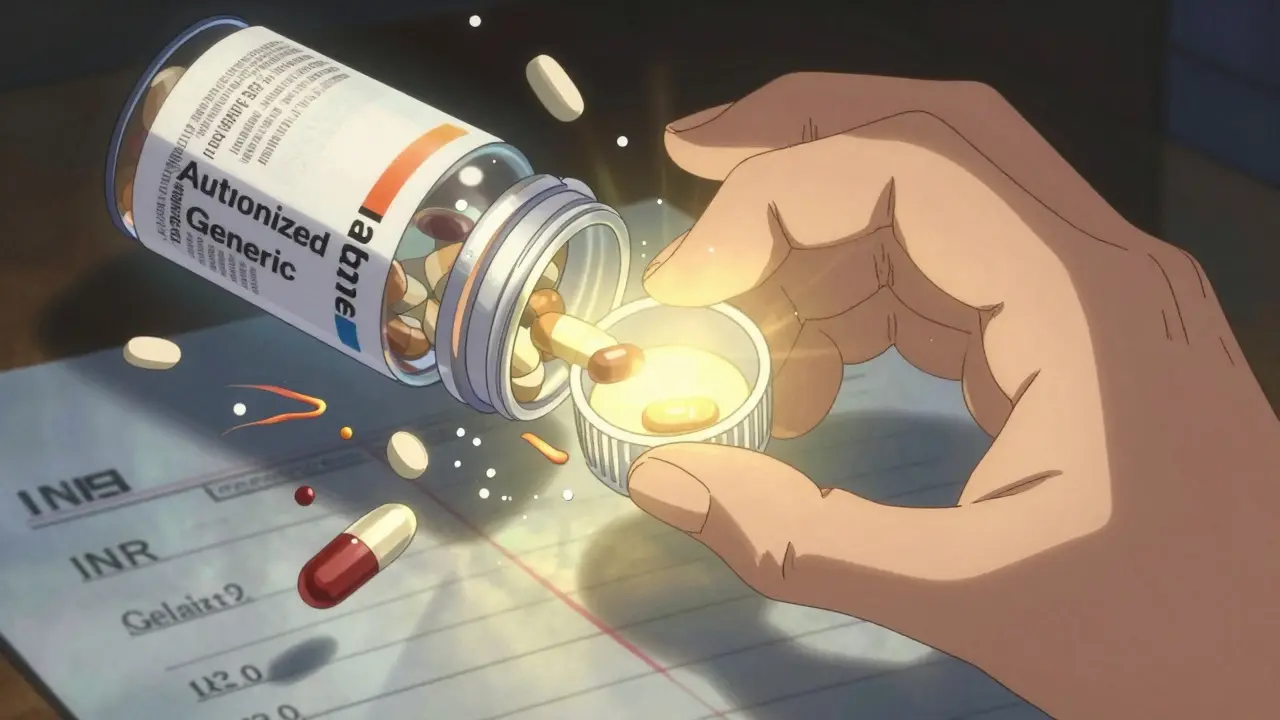
Cost and Insurance: The Hidden Catch
Authorized generics are usually 20-80% cheaper than the brand. That’s huge. But here’s the twist: insurance companies don’t always treat them like generics.
According to a 2022 analysis, 63% of pharmacy benefit managers (PBMs) place authorized generics in the brand-name tier. That means a patient might pay $50 out-of-pocket for an authorized generic, even though it’s chemically identical to a $10 regular generic.
Always check the patient’s formulary. Ask the pharmacy tech to run the NDC through the system. If the copay is sky-high, explain why: “This is the same pill as the brand, but your plan treats it like one.” Then offer alternatives-maybe a regular generic is still safe, or maybe the patient qualifies for a manufacturer discount.
What to Tell Patients
Patients get confused when their pill changes color or shape. A white tablet becomes a blue one. They panic. They stop taking it. A 2022 study found that 27% of patients discontinued therapy after an unexpected appearance change-unless they were properly counseled.
Here’s what to say:
- “This pill looks different, but it’s the same medicine your doctor prescribed. Same active ingredient. Same fillers. Same everything.”
- “It’s made by the same company that makes the brand name. The only difference is the label.”
- “You’ll save a lot of money-often half the price-without changing how it works.”
- “If you’ve had no issues with the brand, this is the safest generic option.”
Don’t assume they understand. Use simple language. Show them the pill. Compare it side-by-side with the old one if possible. This isn’t just education-it’s adherence.

Legal and Regulatory Notes
Pharmacists can substitute an authorized generic unless the prescriber wrote “Do Not Substitute.” That’s true in 42 states. But 18 states require you to notify the prescriber anytime you make a substitution-even for authorized generics.
Always check your state’s pharmacy board rules. Document the substitution with the correct modifier code (usually “DA”) on the claim. Keep a record showing the authorized generic is therapeutically equivalent to the brand-because legally, it is.
And remember: you don’t need prescriber approval to switch to an authorized generic. But you do need to be ready to explain why it’s safe.
What’s Changing in 2025?
The number of authorized generics is growing. Since 2010, availability has increased by 18% per year. More manufacturers are launching them to compete with price wars from generic companies.
Consumer awareness is rising too. GoodRx reports a 47% jump in searches for “authorized generics” between 2021 and 2022. Patients are asking. They’re reading. They’re comparing prices.
Legislation like the Affordable Insulin Now Act of 2023 may expand access to authorized generics for high-cost drugs. Professional groups like the American Pharmacists Association are updating guidelines for 2024 to include clearer recommendations on when to recommend them.
Pharmacists who understand this space won’t just be dispensing pills-they’ll be guiding patients to the safest, most cost-effective option.
Final Thought: It’s Not About Cheapest. It’s About Right.
Generic substitution is standard practice. But “generic” doesn’t always mean “safe.”
For patients with allergies, NTI drugs, or complex formulations, the authorized generic isn’t just an alternative-it’s the best choice. It’s the only option that gives you the brand’s reliability without the brand’s price tag.
Know the list. Know the NDCs. Know your patients. And when in doubt-ask: ‘Is this the same pill they’ve always taken?’ If the answer is yes, then the authorized generic is the answer.