When you pick up a prescription, you might see two names on the bottle: one you recognize, like Norvasc, and another you don’t, like amlodipine. The price difference is huge-$400 for the brand, $2 for the generic. You might wonder: is the cheaper one just as good? Or are you saving money at the cost of your health?
They’re the Same Medicine, Inside
Here’s the simple truth: generic drugs contain the exact same active ingredient as their brand-name counterparts. That means if you’re taking amlodipine for high blood pressure, whether it’s called Norvasc or just amlodipine, your body gets the same molecule. The same goes for metformin instead of Glucophage, sertraline instead of Zoloft, or ibuprofen instead of Advil. The FDA doesn’t allow anything less.
The active ingredient is what makes the drug work. It’s the part that lowers blood sugar, reduces inflammation, or balances brain chemicals. Generic manufacturers must prove they deliver the same amount of that ingredient into your bloodstream at the same speed as the brand-name version. That’s called bioequivalence. The FDA requires it to be within 80% to 125% of the brand’s performance-meaning your body absorbs it nearly identically.
Why Are Generics So Much Cheaper?
Brand-name drugs cost a lot because the company had to pay for years of research, clinical trials, and marketing. They get a patent that lets them be the only one selling it for about 20 years. Once that patent expires, other companies can make the same drug without repeating those expensive studies.
Generics skip the clinical trials because the safety and effectiveness are already proven. All they have to do is show their version works the same way in your body. That cuts development costs by 80% or more. The savings get passed on. According to the Generic Pharmaceutical Association, generics saved the U.S. healthcare system over $300 billion in 2022 alone.
Take metformin, used for type 2 diabetes. The brand Glucophage costs around $350 for a month’s supply. The generic? About $4. That’s not a trick. That’s the system working as designed.
What’s Different? (And Why It Doesn’t Matter)
Generics look different. They might be a different color, shape, or size. They might have a different name printed on them. That’s because trademark laws prevent generics from looking exactly like the brand. But none of that affects how the drug works.
What’s inside the pill-besides the active ingredient-is called an inactive ingredient. These are fillers, binders, dyes, or preservatives. They help the pill hold its shape, dissolve properly, or look appealing. They don’t treat your condition. But they can cause issues for a tiny fraction of people.
For example, someone allergic to a dye used in one generic version of sertraline might get a rash. Or someone with sensitive digestion might feel stomach upset with a different filler. These reactions are rare-less than 0.05% of switches, according to FDA data. If you notice something new after switching, talk to your pharmacist. They can check if it’s the inactive ingredient and find a version without it.
Are Generics Just as Safe and Effective?
Yes. And the science backs it up.
A 2019 study in JAMA Internal Medicine looked at over 3.5 million patients using generics for diabetes, high blood pressure, epilepsy, and depression. The results? No difference in outcomes. Blood sugar levels, blood pressure, seizure control, and depression scores were the same as with brand-name drugs.
Another review in The New England Journal of Medicine analyzed 47 high-quality studies on heart medications. Generics performed just as well. The FDA’s own stance is clear: “Generic drugs work the same as brand-name drugs and are just as effective.”
Even for drugs with a narrow therapeutic index-where small changes in dose can matter, like warfarin or levothyroxine-the FDA requires the same strict bioequivalence standards. Some doctors may prefer to stick with one version for consistency, but that’s about minimizing variables, not because generics are inferior.
Why Do Some People Say Generics Don’t Work for Them?
You’ll find stories online: “I switched to generic sertraline and felt awful.” Or, “My blood pressure spiked after the pharmacy changed my pill.”
These aren’t lies. But they’re often misunderstandings.
First, switching from one pill to another-even if they’re identical in active ingredient-can feel different. Your brain notices the color change. You might start wondering if it’s working. That anxiety can make you feel worse.
Second, if you’ve been on a brand-name drug for years, your body adapts. Switching to a new pill, even an identical one, can cause temporary adjustment symptoms. That doesn’t mean the generic is broken. It just means your body needs a few days to settle.
Third, rare cases do happen. A batch might have a slightly different dissolution rate. Or a new manufacturer’s formulation might not be perfectly matched. But the FDA tracks these. If a pattern emerges, they pull the product and investigate.
Most people-87%, according to a GoodRx survey-report no difference at all. And those who do usually find a different generic version that works better.
What About Complex Drugs? Inhalers, Creams, Injectables?
For simple pills, the rules are clear. But for complex drugs-like inhalers, topical creams, or injectables-it’s harder to prove exact equivalence. That’s why these are often called “biosimilars” instead of generics.
Biosimilars are for biologic drugs, which are made from living cells. They’re more complicated than chemical pills. Even small changes in production can affect how they work. That’s why they go through a more rigorous approval process.
But even here, the goal is the same: match the brand’s effect. The FDA approves them only after showing they’re “highly similar” with no meaningful differences in safety or effectiveness. For most patients, biosimilars are a safe, cheaper option.
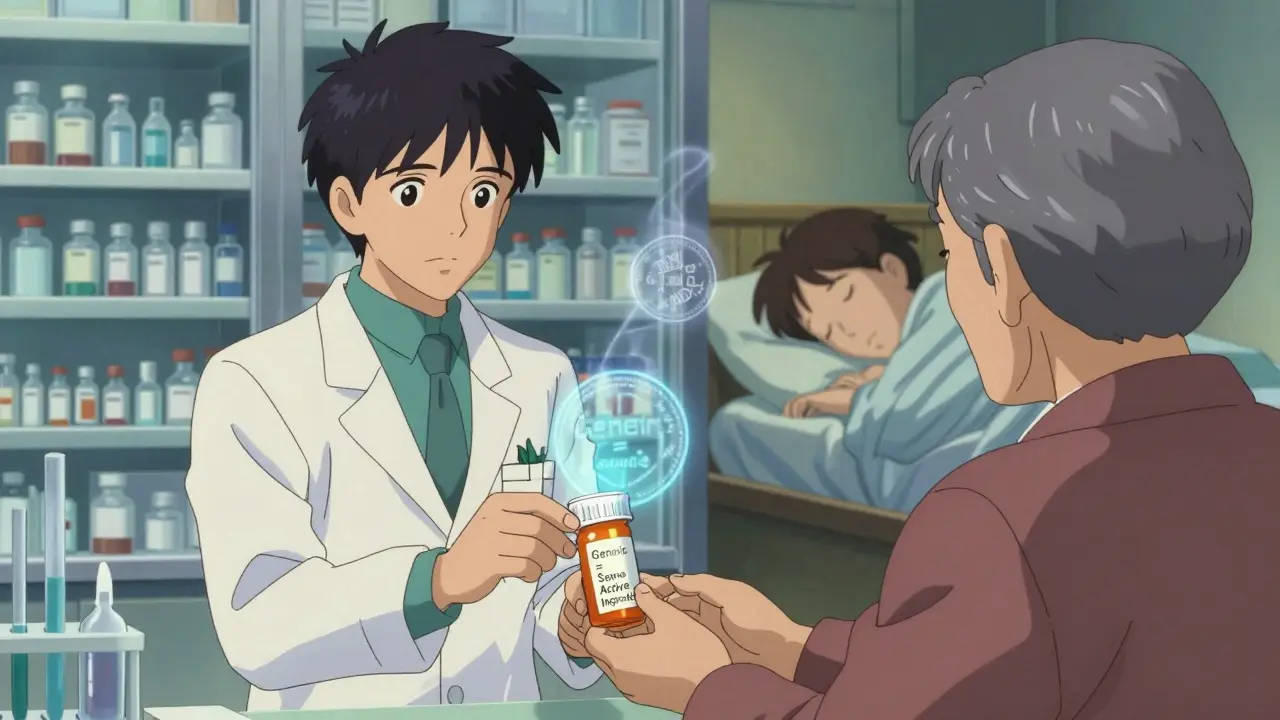
Can Your Pharmacist Switch Your Prescription Automatically?
In 49 U.S. states, yes. Pharmacists can substitute a generic unless the doctor writes “dispense as written” or “no substitution.” This is standard practice.
Insurance companies often require it. If you ask for the brand-name drug when a generic is available, your copay might jump from $5 to $50. That’s not a punishment-it’s an incentive to save money for everyone.
Pharmacists are trained to explain this. A two-minute chat can clear up most concerns. Most patients understand after hearing the facts: same active ingredient, same effect, way cheaper.

Who Makes These Generics?
Generics aren’t made in some shady basement. They’re made by companies like Teva, Mylan, Sandoz, and dozens of others. Many of these manufacturers also make brand-name drugs. The same factories, under the same rules.
The FDA inspects all drug facilities-brand and generic alike-with the same strict standards called cGMP (current Good Manufacturing Practices). In 2022, they inspected over 3,500 facilities worldwide. If a plant fails, it’s shut down.
There have been quality issues-some plants in India and China were flagged in 2022. But those represent less than 0.5% of total production. The FDA tracks every batch. If there’s a problem, they issue alerts and remove products.
What Should You Do?
Here’s what you can do right now:
- Ask your pharmacist: “Is there a generic for this?”
- If you’re switching, pay attention for a few days. Note any new side effects.
- If something feels off, don’t stop taking it. Call your doctor or pharmacist. They can check if it’s the generic, the dose, or something else.
- Use tools like GoodRx to compare prices. Sometimes two different generics cost different amounts.
- Keep your medication list updated. If your pill changes color or shape, make sure you know why.
Most people save hundreds or even thousands of dollars a year by switching. And they get the same results.
Bottom Line
Generics aren’t cheaper because they’re worse. They’re cheaper because they don’t need to pay for advertising, research, or patents. The active ingredient is identical. The effect is identical. The safety standards are identical.
The only real difference? The price tag.
If you’re on a brand-name drug and wondering whether you could save money, ask. It’s not a risk. It’s a smart choice backed by science, regulators, and millions of patients who’ve made the switch without a hitch.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict safety and quality standards as brand-name drugs. All manufacturers-whether making generics or brands-must follow the same current Good Manufacturing Practices (cGMP). The FDA inspects both types of facilities with equal rigor.
Why do generic pills look different from brand-name ones?
By law, generics can’t look exactly like the brand-name version to avoid trademark infringement. That’s why the color, shape, or size might be different. But the active ingredient, strength, and how it works in your body are identical. The differences are only in inactive ingredients like dyes or fillers, which don’t affect the drug’s effectiveness.
Can I trust generics for serious conditions like heart disease or epilepsy?
Absolutely. Large studies involving millions of patients have shown that generics for heart disease, epilepsy, diabetes, and depression work just as well as brand-name drugs. Even for drugs with a narrow therapeutic index-like warfarin or levothyroxine-the FDA requires the same bioequivalence standards. Doctors may recommend sticking with one version for consistency, but that’s not because generics are less reliable.
What if I feel worse after switching to a generic?
It’s rare, but it can happen. Sometimes, the change in inactive ingredients-like a different filler or dye-can cause mild side effects, such as stomach upset. Or, your body might just need time to adjust to a new pill shape or size. If you feel worse, don’t stop the medication. Talk to your pharmacist. They can check if a different generic version is available or if the issue is unrelated.
Do insurance companies force me to use generics?
Many do, because generics are far cheaper. If a generic is available, your insurance may require you to try it first. If you need the brand-name drug, your doctor can write “dispense as written” on the prescription. But in most cases, the generic will work just as well-and save you money.
Most people who switch to generics report no issues. In fact, because generics are affordable, patients are more likely to take their meds regularly-leading to better health outcomes. For chronic conditions like high blood pressure or diabetes, that consistency can mean the difference between staying healthy and ending up in the hospital.