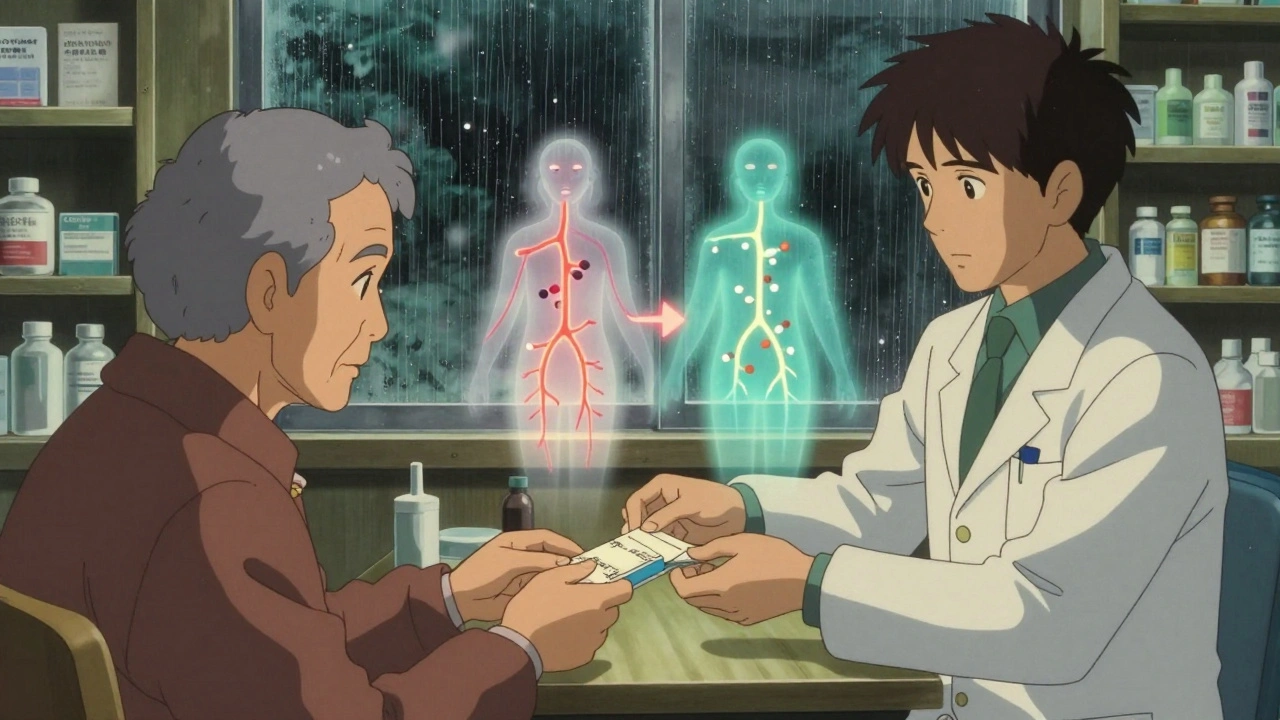
When you pick up a prescription, you might not notice the difference between the brand-name pill and the generic version sitting in your hand. They look different. They cost less. But do they work the same? That’s where therapeutic equivalence comes in - and it’s one of the most important, yet least understood, safeguards in modern medicine.
What therapeutic equivalence actually means
Therapeutic equivalence isn’t just about having the same active ingredient. It’s not even just about matching the dose. It means two drugs - one brand-name, one generic - will do the exact same thing in your body, at the same speed, with the same safety record. The U.S. Food and Drug Administration (FDA) uses strict science to prove this. If a generic drug passes all the tests, it gets an “A” rating in the FDA’s Orange Book, meaning it’s considered interchangeable without any risk to your health.This isn’t guesswork. It’s backed by hard data. For a generic to be rated therapeutically equivalent, it must meet three standards: pharmaceutical equivalence, bioequivalence, and proven clinical outcomes. Pharmaceutical equivalence means identical active ingredients, same dosage form (tablet, capsule, injection), and same strength. Bioequivalence is the real test: the generic must absorb into your bloodstream at the same rate and to the same extent as the brand. The FDA requires the 90% confidence interval for absorption (measured by AUC and Cmax) to fall between 80% and 125%. For high-risk drugs like warfarin or levothyroxine, that range tightens to 90-110%.
What this means for you: if your doctor prescribes Lipitor and your pharmacist gives you atorvastatin with an “AB” rating, you’re getting the same drug, the same way, with the same results. No hidden surprises.
Why this matters for your safety
Patient safety doesn’t just mean avoiding side effects. It means avoiding unexpected side effects. When you switch from one drug to another, even if they’re chemically identical, small differences in how your body absorbs it can cause big problems - especially with drugs where the difference between effective and toxic is razor-thin.Take thyroid medication. Levothyroxine has a narrow therapeutic index. A 5% change in absorption can throw your hormone levels off. That’s why the FDA requires tighter bioequivalence standards for it. If a generic fails to meet those tighter limits, it doesn’t get an “A” rating. It gets a “B” - meaning it’s not recommended for automatic substitution. Pharmacists are trained to spot these. And if you’re on one of these drugs, your pharmacist should flag any switch.
Between 2018 and 2022, the Institute for Safe Medication Practices recorded 127 adverse events tied to generic substitution. Only 17 involved drugs with an “A” therapeutic equivalence rating. The rest? Either non-equivalent generics, drugs switched without proper evaluation, or cases where patient anxiety - not the drug - caused the issue. The data is clear: when therapeutic equivalence is properly applied, safety isn’t compromised. It’s protected.
How the FDA’s Orange Book keeps you safe
The FDA’s Orange Book is the official database that lists every drug approved in the U.S. and marks which ones are therapeutically equivalent. It’s updated every month. As of October 2023, it includes over 13,000 drug products. Each entry has a two-letter code:- A = Therapeutically equivalent. Safe to substitute.
- B = Not equivalent. Don’t swap without checking.
The second letter adds more detail - like whether it’s an immediate-release (AB), extended-release (AX), or a product with special formulation issues (AP, AR). Pharmacists use this code every time they fill a prescription. If your script says “atorvastatin 20 mg” and the Orange Book shows “AB,” your pharmacist can legally swap it for the generic without asking your doctor. In 49 U.S. states, they’re even required to do so unless you or your doctor say no.
This system saves billions. From 2009 to 2019, generic drugs saved the U.S. healthcare system $1.7 trillion. In 2022 alone, generics made up 90.7% of all prescriptions dispensed - but only 58% of total drug spending. That’s not just cost savings. It’s access. Without therapeutic equivalence, many people couldn’t afford their meds at all.
What about those stories of problems after switching?
You’ve probably heard them. Someone switched to a generic and felt weird. Their blood pressure spiked. Their pain came back. They blamed the generic. But here’s what rarely gets said: most of those cases aren’t caused by the drug.A 2022 UnitedHealthcare survey of 12,500 patients found 87% reported no change in how they felt after switching to an Orange Book-listed generic. Only 3.2% reported adverse effects they thought were linked to the switch. When researchers looked closer, most of those cases involved drugs with “B” ratings - or were actually therapeutic interchanges (switching from one class of drug to another, like from one statin to a different one), not true therapeutic equivalents.
On Reddit’s r/pharmacy thread from August 2021, 47 people reported issues after switching. Only 3 involved products with “A” ratings. The rest? Non-equivalent generics, mislabeled products, or patients who didn’t realize they were switched at all.
Human psychology plays a role too. If you believe a generic is “less effective,” your brain can amplify minor side effects. That’s not the drug’s fault - it’s the expectation. But therapeutic equivalence removes that uncertainty. When you know the drug has passed the same rigorous tests as the brand, you can trust it.
Where therapeutic equivalence falls short
It’s not perfect. Some drugs are too complex to measure with standard blood tests. Inhalers, topical creams, eye drops, and injectables like insulin can behave differently even if their active ingredient matches. The FDA admits this. For these, bioequivalence studies using traditional methods often don’t work.In November 2023, the FDA released draft guidance for complex products like topical corticosteroids. They’re now using advanced methods - like imaging, in vitro testing, and real-world outcome tracking - to evaluate equivalence. That’s good news. But it’s still evolving. If you’re on an inhaler or a medicated cream, ask your pharmacist: “Is this rated as therapeutically equivalent in the Orange Book?” If they can’t answer, it might not be.
Biosimilars are another gray area. They’re not generics. They’re not identical. They’re “similar enough.” The FDA gives them an “interchangeability” designation - a separate category from therapeutic equivalence. Don’t assume a biosimilar is automatically interchangeable. Always check the label.

What you can do to stay safe
You don’t need to be a pharmacist to protect yourself. Here’s what works:- Know your drug’s rating. Ask your pharmacist: “Is this generic rated AB in the Orange Book?”
- Don’t assume all generics are the same. If you’re on a narrow therapeutic index drug (warfarin, levothyroxine, phenytoin, digoxin), stick with the same brand or generic unless your doctor approves a switch.
- Track how you feel. If you notice new side effects, fatigue, or changes in symptoms after a switch, write them down and call your doctor. Don’t ignore it.
- Check your prescription label. If it says “Dispense as Written” or “Do Not Substitute,” your doctor is telling the pharmacist not to switch. Honor that.
- Use the FDA’s Orange Book. It’s free and public. Search by brand or generic name. If it says “A,” you’re good.
Therapeutic equivalence isn’t a marketing slogan. It’s science. It’s regulation. It’s the reason millions of people can afford their meds without risking their health. When done right, it’s one of the safest, smartest systems in medicine.
What’s next for therapeutic equivalence?
The FDA is investing in new tools. A $2.3 million project with MIT is using artificial intelligence to predict which generic formulations might cause problems before they even hit the market. GDUFA III, a funding program running through 2027, is putting $65 million into better testing for complex drugs. The goal? To expand therapeutic equivalence to more drug types - safely.Meanwhile, doctors and pharmacists are getting better training. The FDA’s free 90-minute online course has helped 85% of participants improve their ability to spot safe substitutions. That’s progress.
Therapeutic equivalence will keep evolving. But its core mission won’t change: make safe, affordable medicine accessible - without compromise.
Are generic drugs as safe as brand-name drugs?
Yes - if they’re rated therapeutically equivalent by the FDA. Generic drugs must prove they deliver the same active ingredient at the same rate and extent as the brand. The FDA requires strict bioequivalence testing, and only drugs that pass get an “A” rating. Millions of people use these daily without issue. The safety record is strong.
What does an “AB” rating mean on the FDA Orange Book?
An “AB” rating means the drug is considered therapeutically equivalent to the brand-name product. The “A” means it’s interchangeable; the “B” means it’s not. “AB” specifically refers to immediate-release oral products that have passed bioequivalence testing. You can safely substitute an “AB” generic for the brand.
Can I switch between different generic versions of the same drug?
If both generics have an “AB” rating, yes - they’re considered equivalent. But if you’re on a narrow therapeutic index drug like warfarin or levothyroxine, switching between different generics - even if both are rated AB - can sometimes cause small changes in how your body responds. Talk to your doctor before switching, even between two approved generics.
Why do some generics cost more than others?
Price differences between generics usually come from manufacturing costs, supply chain issues, or how many companies make the drug. If only one company makes a generic, it can charge more. But if multiple companies make the same drug, competition drives prices down. Cost doesn’t reflect safety or effectiveness - only the Orange Book rating does.
Do I need to tell my doctor if I switch to a generic?
You don’t have to - unless you notice a change in how you feel. Therapeutic equivalence means the switch should be seamless. But if you experience new side effects, worsening symptoms, or unexpected reactions after switching, contact your doctor. It’s always better to report changes than to assume they’re normal.