OTC Medication Safety Checker
Check potential interactions between your medications and OTC products. Enter your current medications, health conditions, and age to see if there are any safety concerns.
Medication Safety Assessment
When a medication moves from prescription-only to over-the-counter (OTC), it’s not just a change in where you buy it-it’s a shift in how you use it. You no longer need a doctor’s note. You can grab it off the shelf like pain relievers or antacids. But that convenience comes with risks most people don’t think about. In 2023, more than 100,000 OTC products were available in the U.S. alone. And while this change saves time and money, it also means you’re now responsible for knowing what you’re taking, how much, and whether it’s safe with your other meds. This isn’t just about headaches or colds. It’s about your liver, your kidneys, your heart.
Why Do Drugs Switch from Prescription to OTC?
The idea behind switching a drug from prescription to OTC is simple: if it’s safe enough for people to use without a doctor, why make them wait? The U.S. Food and Drug Administration (FDA) only approves these switches after years of data showing the drug works as claimed and doesn’t cause serious harm when used as directed. For example, ibuprofen was a prescription drug until 1984. Back then, a month’s supply cost $30-$40. After the switch, it dropped to $5-$10. That’s a huge win for consumers-and for the healthcare system, which avoids millions of unnecessary doctor visits every year.
But here’s the catch: just because it’s easier to get doesn’t mean it’s harmless. The FDA looks at three things before approving a switch: Can you self-diagnose the problem? Can you follow the label without help? And is the drug safe enough that even if you misuse it a little, you won’t end up in the hospital? If the answer is yes to all three, the switch happens. But real life doesn’t always match the lab.
The Hidden Dangers of Self-Medication
Most people think OTC means “safe.” But that’s not true. OTC drugs are powerful chemicals. Take acetaminophen-the active ingredient in Tylenol. It’s fine at 650 mg every 6 hours. But take two different cold medicines, and you might be getting 1,000 mg from one and 500 mg from the other. That’s 1,500 mg in one day. The safe daily limit is 3,000 mg. Sounds fine, right? Except if you drink alcohol, have liver disease, or take other meds, that limit drops to 2,000 mg. And if you keep going? Liver failure. It doesn’t happen overnight. It creeps up. By the time you feel sick, it’s too late.
NSAIDs like ibuprofen and naproxen are another silent threat. They’re great for pain and inflammation. But take them for more than 10 days in a row without knowing why your pain started? You could be damaging your stomach lining, kidneys, or even increasing your risk of a heart attack or stroke. The FDA warns that these risks go up the longer you use them-and most people don’t track how long they’ve been taking them.
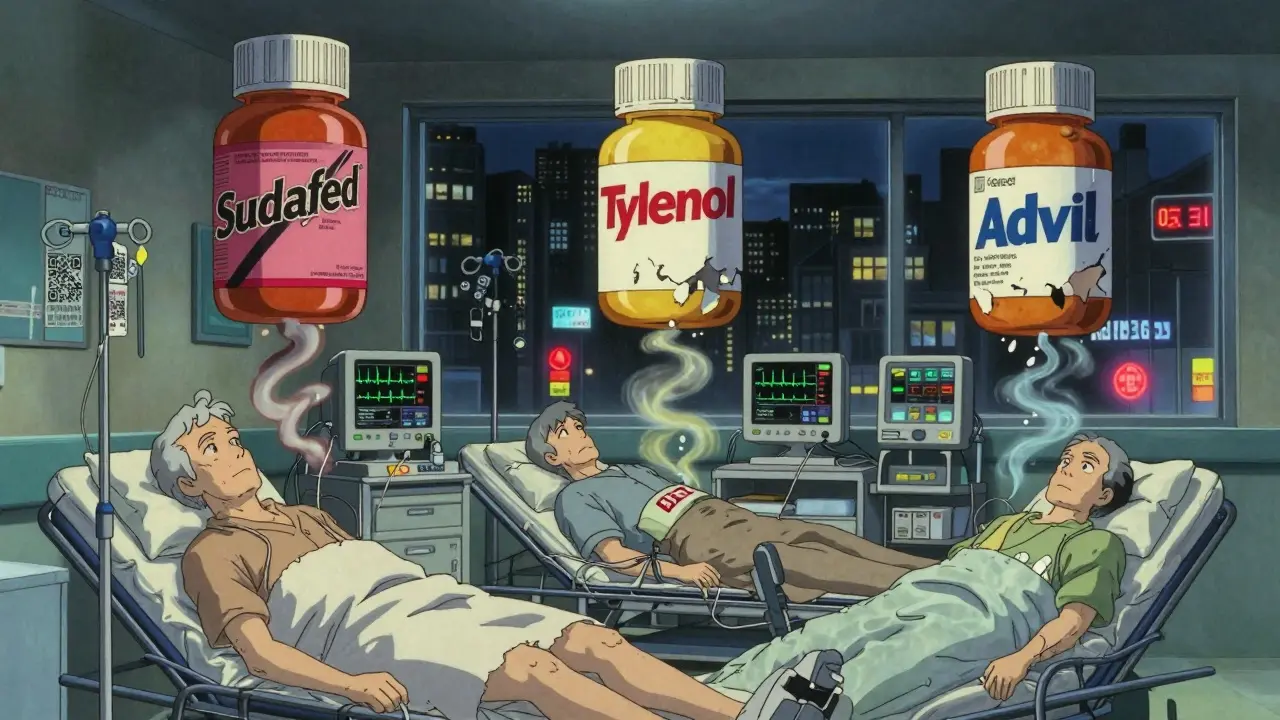
And then there’s pseudoephedrine, the decongestant in Sudafed. It’s been behind-the-counter since 2005 because it’s used to make meth. But even if you’re not making drugs, it can spike your blood pressure dangerously high if you’re on certain antidepressants or blood pressure meds. One 2022 Reddit post from a nurse described multiple elderly patients who ended up in the ER after starting OTC decongestants while already on hypertension meds. They didn’t think it mattered. They were just trying to clear their sinuses.
Who’s Most at Risk?
Not everyone handles OTC drugs the same way. Older adults are especially vulnerable. As we age, our bodies process drugs slower. That means even a normal dose can build up. The American Geriatrics Society has a list called the Beers Criteria-it names 30 OTC drugs that are risky for people over 65. One of them? Diphenhydramine, the sleepy ingredient in Benadryl. It can cause confusion, dizziness, and falls. Another? Long-term NSAID use, which doubles or even quadruples the risk of stomach bleeding in seniors.
People taking three or more medications are also at high risk. If you’re on a blood thinner, a diabetes pill, and a heart medication, adding an OTC pain reliever or sleep aid can create a dangerous mix. The FDA says OTC drugs can make your prescriptions less effective-or worse, cause reactions you didn’t expect. For example, mixing antihistamines with alcohol can make you pass out. Taking dextromethorphan (a cough suppressant) with certain antidepressants can trigger serotonin syndrome-a rare but life-threatening condition.
And then there’s the knowledge gap. A 2023 study in Bangalore found that 77% of people didn’t know the contraindications of their OTC meds. Only 13% could name possible side effects. And pharmacists? Many didn’t ask about existing conditions or allergies. That’s not just negligence-it’s a systemic failure.
What You Need to Do Before Taking Anything
You can’t rely on luck. You need a system. Here’s what to do every time you pick up an OTC drug:
- Read the Drug Facts label. It’s not just fine print. It’s your safety guide. Look for the active ingredient first. Then check the warnings. If it says “Do not use if you have high blood pressure,” and you have high blood pressure, put it back.
- Cross-check all your meds. Write down every pill, patch, or liquid you take-even vitamins and herbal supplements. Then compare active ingredients. If two products have the same one (like acetaminophen or ibuprofen), you’re doubling up. That’s how liver damage happens.
- Ask the pharmacist. Not the cashier. The pharmacist. They’re trained to spot interactions. Tell them what you’re taking, what you’re feeling, and how long you’ve been taking it. Even if you think it’s “just an OTC,” they’ve seen the mistakes before.
And if you’re over 65, or have kidney, liver, heart, or lung problems? Don’t guess. Talk to your doctor before trying anything new-even if it’s been OTC for 20 years.
What’s Changing? The Future of OTC Safety
Regulators are trying to catch up. The FDA launched a new label design in 2022 with bigger fonts, clearer warnings, and simpler language. They’re also pushing companies to add QR codes to packaging that link to updated safety info, drug interaction checkers, and video tutorials. Walmart started testing this in 2023 on 15% of its private-label OTC products. It’s a start.
But technology won’t fix human behavior. The biggest danger isn’t bad drugs-it’s bad habits. People don’t realize OTC meds are still drugs. They think, “It’s just aspirin,” or “I’ve taken this for years.” But your body changes. Your other meds change. Your health changes. And what was safe last year might not be safe today.
Experts agree: the line between self-care and self-harm is thin. Dr. Michael Ruffin, a family physician, says it best: “Anytime you take medicine, be aware of changes in your body and how you feel. Tell your doctor when the symptom started.” Because sometimes, what feels like a cold is something worse. And what feels like a harmless OTC fix might be making it worse.
Final Thought: OTC Doesn’t Mean Risk-Free
OTC switches give you freedom. But freedom without knowledge is dangerous. You have more control now than ever before. But that means you also have more responsibility. Don’t treat OTC meds like candy. Don’t assume they’re safe because they’re on a shelf. Read the label. Know your meds. Talk to a pharmacist. And if you’re unsure? Call your doctor. It’s not a sign of weakness. It’s the smartest thing you can do.