Every parent knows the panic of seeing a rash on their child’s skin. Maybe it’s eczema flaring up, a bug bite that won’t quit, or a diaper rash that won’t respond to plain zinc oxide. It’s tempting to grab the nearest cream - even one that worked for you - and slap it on. But what’s safe for adults can be dangerous for kids. Topical medications for children aren’t just weaker versions of adult products. They demand precision, caution, and a deep understanding of how a child’s body absorbs them differently.
Why Children’s Skin Is Not Just Smaller Skin
A baby’s skin isn’t just tiny adult skin. It’s thinner, more porous, and still learning how to protect itself. By the time a child is one year old, their skin absorbs topical medications 3 to 5 times more easily than an adult’s. For newborns? That number jumps even higher. This isn’t theory - it’s physiology. The outer layer of skin, called the stratum corneum, is still developing. That means chemicals don’t just sit on the surface. They slip right through.
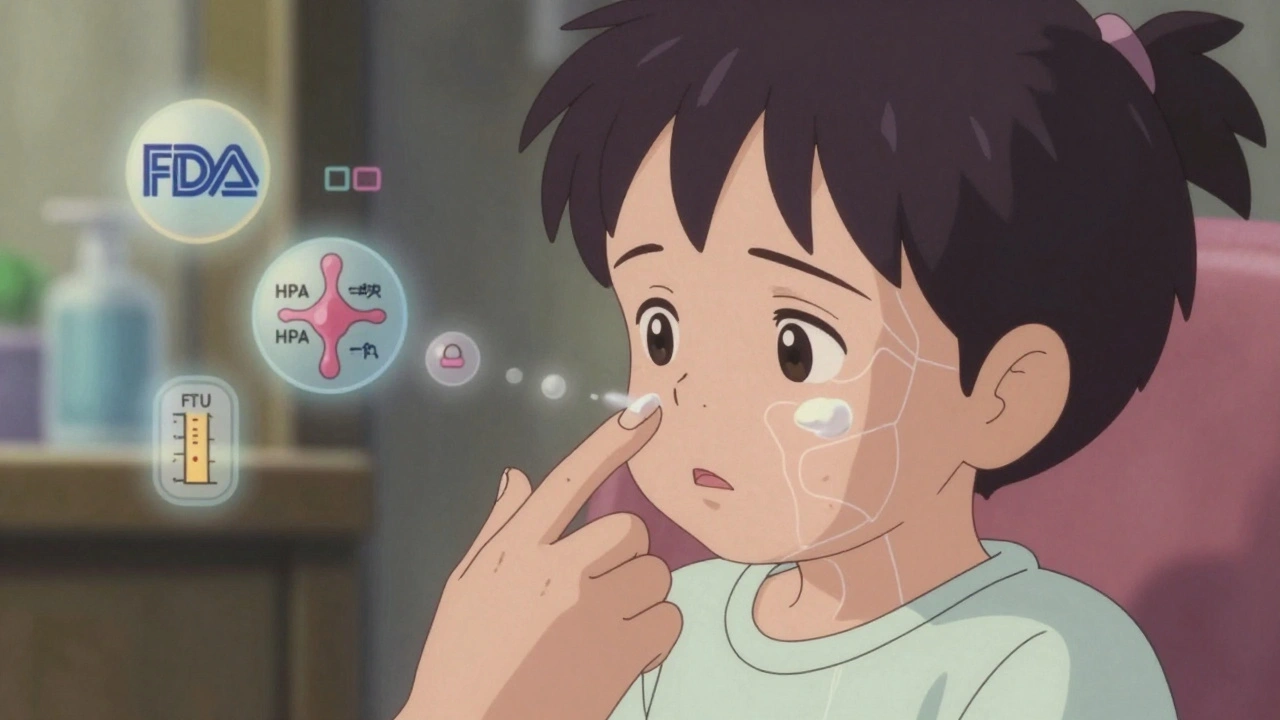
That’s why a pea-sized dab of hydrocortisone on a toddler’s arm might be fine. But the same amount spread across 20% of an infant’s body - say, both legs and the back - can suppress their stress hormone system. That’s the HPA axis. It’s the same system that gets knocked out by oral steroids. And yes, it can happen from a cream you thought was harmless.
The Hidden Dangers: What Not to Use
Some of the most common over-the-counter products are the most dangerous for young children. Benzocaine, found in teething gels and numbing sprays, is a silent killer. It doesn’t cause vomiting or fever. It causes methemoglobinemia - a condition where blood can’t carry oxygen. Babies can go from fussy to blue-lipped and breathing hard in under 30 minutes. Since 2006, more than 400 cases have been documented in children under two. The FDA banned these products for infants under two for a reason.
Another big no: dibucaine and high-strength lidocaine creams. While lidocaine is safe in controlled medical settings - like before a needle - using it at home for diaper rash or sunburn? Risky. On broken skin, absorption can spike from 3% to 60%. That’s enough to trigger seizures in a small child. The American Academy of Pediatrics doesn’t recommend routine use in babies under 12 months.
And then there’s the corticosteroid trap. Many parents grab their own hydrocortisone cream from the bathroom cabinet. But not all are created equal. Class I steroids (like clobetasol) are for severe psoriasis in adults - not for a toddler’s cheek. Even low-potency hydrocortisone (Class VII) can cause problems if used too often, too widely, or under occlusion. Occlusion means covering the area with plastic wrap, Tegaderm, or even a tight onesie. That can boost absorption by 300-500%. In infants with eczema, that’s a recipe for adrenal suppression.
What’s Actually Safe - And How to Use It
Good news: there are safe, effective options. For eczema, the American Academy of Pediatrics now recommends topical calcineurin inhibitors like tacrolimus (0.03%) or pimecrolimus as first-line for facial and sensitive areas in children over 3 months. These work just as well as low-dose steroids - without the HPA axis risk. Yes, the FDA has a black box warning about cancer risk. But after 15 years of real-world use, not a single confirmed case has been linked to these creams. The risk is theoretical. The benefit is real.
For mild rashes or irritation, plain moisturizers are often the best medicine. Look for fragrance-free, ceramide-based creams. They repair the skin barrier - the root cause of most childhood eczema. For teething, skip the gel. Try a chilled (not frozen) silicone teether. Cold numbs. Ice can damage tissue. Frozen items are too hard and risk choking.

The Fingertip Unit: Your Secret Weapon for Dosing
Most parents don’t know how much cream to use. “A pea-sized amount” sounds vague. And it is. The medical standard is the fingertip unit (FTU). One FTU is the amount of cream squeezed from a standard tube, from the tip of the index finger to the first crease. That’s about 0.5 grams.
One FTU covers an area equal to two adult palms - flat, fingers together. For a 10kg child (about 22 pounds), the maximum daily dose of a low-potency steroid should be no more than 2 grams total - that’s four FTUs. And you shouldn’t treat more than 10% of the body surface at once. That means: one FTU for the face and neck, one for each arm, one for each leg. That’s it.
Using more doesn’t make it work faster. It just increases the risk of side effects. And never apply it to broken, oozing, or infected skin. That’s when absorption spikes. Always use it on clean, dry skin. Wait 15 minutes before putting on clothes or diapers.
Storage and Prevention: Keep It Out of Reach - Even When You’re Using It
Most accidental poisonings happen not because kids found the medicine cabinet, but because the tube was left on the changing table, the sink, or the nightstand while you were applying it. The American Association of Poison Control Centers says 78% of pediatric topical medication exposures happen this way.
Always put it back in the child-resistant container - immediately. Don’t leave it out while you’re answering the phone, feeding the baby, or checking your phone. That’s the moment it happens. The CPSC made child-resistant packaging mandatory for prescription anesthetics in 1994. But many OTC products still slip through. Check the label. If it doesn’t have a safety cap, don’t use it.

When to Call for Help
Most reactions aren’t obvious. But if your child becomes unusually sleepy, has trouble breathing, develops a bluish tint to their lips or fingers, or starts having seizures after you applied a cream - call 911 or your poison control center immediately. Methemoglobinemia from benzocaine can be reversed with methylene blue - but only if treated fast.
Don’t wait for symptoms to get worse. If you’re unsure whether a product is safe, call the FDA’s Division of Drug Information at 1-855-543-3784. They’ll tell you if it’s approved for children and what the risks are.
The Bigger Picture: Why This Matters
Topical medication errors send about 6,500 children under five to U.S. emergency rooms every year. That’s not just a statistic. That’s a parent’s worst nightmare. And it’s preventable.
The market for pediatric topical products is growing - $18.7 billion by 2027. But safety isn’t keeping up. In India, 78% of steroid creams are sold without a prescription. In the U.S., over a third of OTC lidocaine products still don’t meet child-resistant packaging standards. And many parents still use adult creams on kids because “it’s just a little bit.”
The solution isn’t more drugs. It’s better education. It’s knowing that less is more. That a cream isn’t a quick fix - it’s a tool. And like any tool, it can hurt if used wrong.
What You Can Do Today
- Never use benzocaine or lidocaine on infants under two.
- Always use the fingertip unit - never guess the amount.
- Never apply topical steroids under plastic wrap or tight clothing unless your doctor says so.
- Store all creams in child-resistant containers, out of reach - even during use.
- Use moisturizers first. Medications second.
- Ask your pediatrician: “Is this safe for my child’s age? What’s the maximum daily dose?”
Children’s skin is delicate. Their bodies are still growing. What feels like a small act - a quick swipe of cream - can have big consequences. Treat topical medications like you would a prescription pill: with care, clarity, and respect.
Can I use my hydrocortisone cream on my baby’s rash?
Only if it’s low-potency (1% hydrocortisone) and approved by your pediatrician. Never use stronger versions. Apply only to small areas, no more than twice a day, and never for longer than 7 days. Avoid using it on the face unless directed. Always use the fingertip unit - one FTU covers two adult palms. If the rash doesn’t improve in 3-4 days, stop and see a doctor.
Is it safe to use topical lidocaine for teething pain?
No. The FDA explicitly warns against all topical anesthetics like lidocaine and benzocaine for teething. They can cause seizures or methemoglobinemia - a life-threatening blood condition. The risk is highest in babies under two. Use a chilled (not frozen) silicone teether instead. Cold reduces swelling and numbs gently without chemicals.
What should I do if my child swallows a topical cream?
Call poison control immediately - even if your child seems fine. Do not wait for symptoms. If it’s a steroid or anesthetic, symptoms like drowsiness, blue skin, or trouble breathing can appear within minutes. Keep the product container handy - the ingredients matter. In the U.S., call 1-800-222-1222. Do not try to make your child vomit unless instructed by a professional.
Are natural or organic creams safer for kids?
Not necessarily. “Natural” doesn’t mean safe. Many plant oils, essential oils, and herbal extracts can irritate infant skin or cause allergic reactions. Some contain compounds that act like steroids or anesthetics without being labeled as such. Always check the ingredient list. Avoid camphor, eucalyptus, tea tree oil, and menthol in children under two. Stick to fragrance-free, hypoallergenic moisturizers with ceramides - they’re the safest choice.
How do I know if a topical medication is approved for my child’s age?
Look for the “Pediatric Use” section on the label. Prescription products must list approved ages and dosing. For over-the-counter products, check the FDA website or call their helpline at 1-855-543-3784. If the label says “for adults” or doesn’t mention children, assume it’s not safe. Never use a product past its expiration date - potency changes, and ingredients can break down into harmful compounds.
Can I share my child’s cream with another child?
Never. Even if the symptoms look the same, children have different weights, skin conditions, and sensitivities. A cream that’s safe for your 18-month-old could be dangerous for a 6-month-old. Sharing medications increases the risk of overdosing and infection. Always use only what’s prescribed or recommended for your child - and never let others use it.