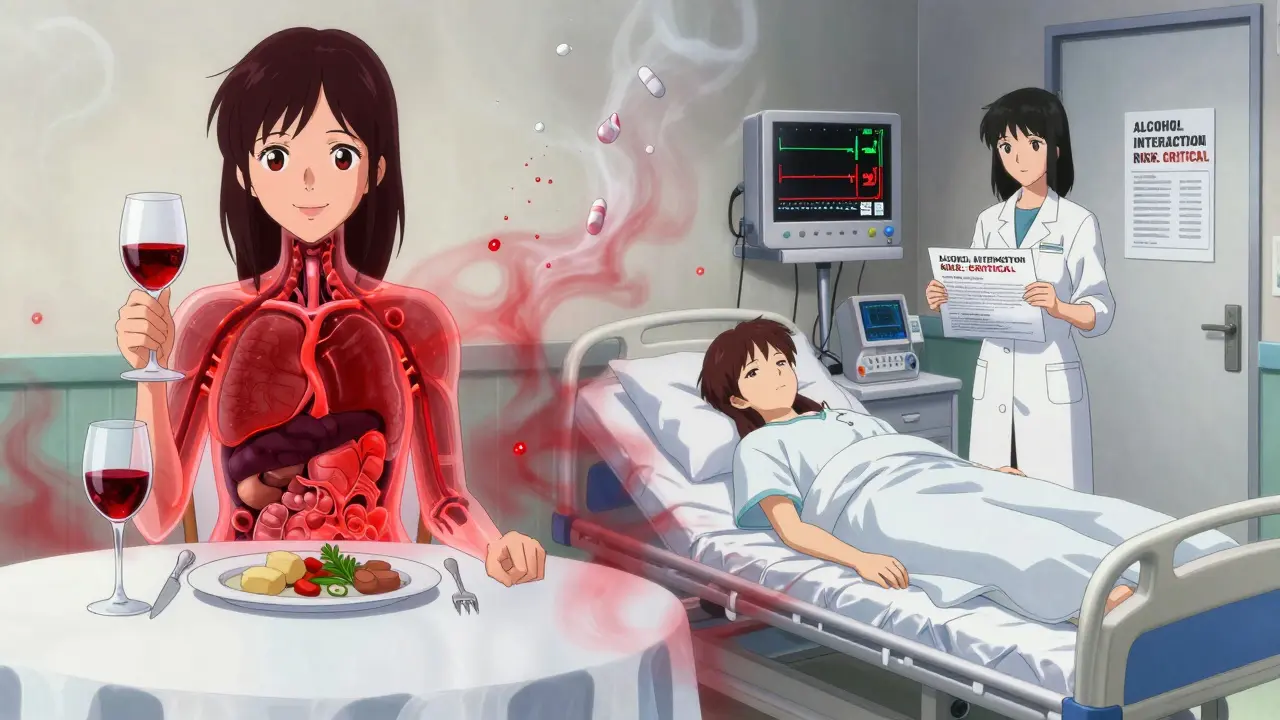
When you take a pill for your blood pressure, anxiety, or pain, you might not think about what happens when you have a glass of wine, a beer, or a shot of whiskey. But mixing alcohol with medications is far more dangerous than most people realize. In fact, alcohol and medication interactions are one of the most common causes of preventable hospital visits in the U.S., with over 2,000 cases reported each year. And here’s the thing-many people don’t even know they’re at risk.
How Alcohol and Medications Fight Inside Your Body
Your liver doesn’t treat alcohol and pills the same way. Both need to be broken down by enzymes, especially a group called cytochrome P450. When alcohol and medication are in your system at the same time, they compete for space. This isn’t just a traffic jam-it can cause serious problems.There are two main ways this goes wrong:
- Pharmacokinetic interactions: Alcohol changes how fast your body processes the drug. If you drink right after taking a pill, alcohol can slow down its breakdown. That means the drug builds up in your blood-sometimes 25% to 75% higher than it should be. That’s like taking double your dose without realizing it.
- Pharmacodynamic interactions: Alcohol and the drug hit the same part of your body. For example, both benzodiazepines (like Xanax) and alcohol calm your brain. When they team up, they can slow your breathing to dangerous levels-even at low alcohol levels like 0.05% (that’s less than one drink for most people).
Chronic drinking makes it worse. If you drink regularly, your liver starts making more enzymes to handle alcohol. That can make your meds less effective. So your blood pressure medicine might stop working, or your antidepressant might not help as much.
Medications That Are Especially Dangerous With Alcohol
Not all drugs react the same way. Some are okay in small amounts. Others? One drink can land you in the ER.Antibiotics like metronidazole (Flagyl): This one is brutal. Even one drink can cause flushing, nausea, vomiting, and a racing heart. In 92% of cases, the reaction happens fast. People have ended up in the ER after just a sip of wine while on this drug.
Benzodiazepines and sleep aids: Drugs like diazepam (Valium), alprazolam (Xanax), and zolpidem (Ambien) are already meant to make you sleepy. Alcohol turns that into a deep, dangerous sedation. The risk of stopping breathing goes up dramatically. These combinations account for over a third of all alcohol-medication deaths.
Antidepressants: SSRIs like fluoxetine (Prozac) don’t cause the same violent reactions as antibiotics, but they make alcohol hit harder. Studies show people feel drunker, longer-up to 3.2 extra hours of intoxication. That means poor judgment, slower reactions, and a higher chance of accidents.
Acetaminophen (Tylenol): This common painkiller is safe if you take it as directed. But if you drink three or more drinks a day, your liver starts to break down acetaminophen into a toxic chemical. Over time, this can cause liver failure. A 2023 study found 18% of people who mixed even moderate alcohol with Tylenol had signs of liver stress.
NSAIDs like ibuprofen or naproxen: These are common for headaches or arthritis. But when you add alcohol, your stomach lining gets damaged faster. The risk of internal bleeding jumps 300% to 500%. That’s not just an upset stomach-it can be life-threatening.
Opioids: Morphine, oxycodone, hydrocodone-any opioid paired with alcohol is a recipe for respiratory failure. The CDC found the risk of fatal breathing problems increases 8 times when these two are combined.
What About Over-the-Counter Drugs?
People think OTC means safe. It doesn’t.Antihistamines like diphenhydramine (Benadryl) are used for allergies or sleep. But they’re already drowsiness-inducing. Add alcohol, and that drowsiness multiplies by 300%. You might not realize how slow your reactions are until you try to drive-or even stand up.
Even cold and flu medicines often contain alcohol, acetaminophen, or antihistamines. Read the labels. If it says "contains alcohol" or "may cause drowsiness," it’s not worth the risk.

Who’s at the Highest Risk?
It’s not just heavy drinkers. The biggest danger zone is people who take multiple medications and think they’re being careful.- Older adults: As we age, our liver processes alcohol slower. Blood flow to the liver drops by 35% between age 25 and 75. That means drugs and alcohol stick around longer. The American Geriatrics Society lists 17 medications that are especially risky for seniors.
- People on 5+ prescriptions: Nearly 70% of adults over 65 take five or more medications. That’s a perfect storm for hidden interactions.
- Those who don’t talk to their pharmacist: Only 42% of prescription bottles have a clear warning about alcohol. And 68% of patients say their doctor never mentioned it.
Here’s a hard truth: 68% of adults believe it’s safe to have a drink or two with any medication. That’s wrong. Even "moderate" drinking can be dangerous if you’re on the wrong drugs.
What Should You Do?
You don’t have to quit alcohol forever. But you do need to be smart.- Ask your doctor or pharmacist: Don’t assume. Ask: "Is it safe to drink alcohol with this?" Be specific about how much and how often you drink.
- Check your meds: Use tools like the NIAAA’s Alcohol-Medication Interaction Risk Calculator (AMIRC) or GoodRx’s interaction checker. But remember-only 37% of online tools are fully accurate. Always double-check with a professional.
- Know your standard drinks: One drink = 12 oz beer (5% alcohol), 5 oz wine (12%), or 1.5 oz spirits (40%). Anything more is not "one drink."
- Wait 2-3 hours after taking your pill: If you’re on a lower-risk medication, spacing out alcohol and your dose can help. But don’t rely on timing alone.
- Never drink on an empty stomach: Food slows alcohol absorption. That gives your liver more time to process it.
- Stop drinking 72 hours before starting high-risk drugs: For antibiotics like metronidazole, this cuts the reaction risk from 92% to just 8%.
What’s Changing in 2026?
New rules are coming. Starting in January 2024, the FDA required all high-risk medications to include pictograms on labels showing alcohol interaction warnings. Pharmacies are now required to flag potential interactions in their systems before filling prescriptions. Telehealth platforms now ask patients about alcohol use during every virtual visit.And there’s progress on education. Stanford’s AI system, which alerts doctors when a patient is prescribed alcohol-risky meds, cut dangerous combinations by 37% in just six months. But most doctors still aren’t trained on this. Only 39% of medical schools teach alcohol-medication interactions as a separate topic.
That’s why your role matters. If you’re on meds, you’re the first line of defense.
Real Stories, Real Consequences
One woman took a single beer with her metronidazole and ended up in the ER with a heart rate of 180. Another man mixed hydroxyzine (an allergy pill) with wine at his daughter’s wedding-and nearly passed out while standing. His pharmacist had warned him. He ignored it. He was lucky.On the flip side, a 72-year-old man was about to refill his diazepam when his pharmacist asked about his weekend wine habit. They switched his medication. He’s been sober since. "I didn’t know," he said. "Now I do."
Knowledge saves lives. And you don’t need to be a doctor to understand the basics.
Can I have one glass of wine with my medication?
It depends on the medication. For some, like metronidazole or opioids, even one drink is unsafe. For others, like SSRIs or NSAIDs, one drink might be okay if you’re healthy and don’t drink often. But there’s no universal rule. Always check with your pharmacist or doctor. When in doubt, skip it.
Do all prescription labels warn about alcohol?
No. Only 42% of prescription bottles include a specific alcohol warning, according to a 2021 FDA audit. Many patients assume the warning is there, but it’s often missing. Don’t rely on the label. Ask your provider.
Is it safe to drink the day before or after taking medication?
For most medications, yes-but not all. Drugs with long half-lives, like diazepam (Valium), stay in your system for days. If you take it daily, drinking even two days later can still be risky. For short-acting drugs, 24 hours is often enough. But for high-risk drugs like metronidazole, wait 72 hours before and after.
Can alcohol make my medication less effective?
Yes. If you drink regularly, your liver produces more enzymes to break down alcohol. This can speed up the metabolism of some drugs, making them less effective. This is common with antidepressants, blood thinners, and some seizure medications. You might think your treatment isn’t working-but it’s the alcohol that’s interfering.
What should I do if I accidentally mixed alcohol and medication?
If you feel dizzy, nauseous, have trouble breathing, or your heart is racing, call 911 or go to the ER immediately. For milder symptoms like drowsiness or nausea, call Poison Control at 1-800-222-1222. Don’t wait. Even if you feel fine now, reactions can build up hours later.
Are there tools I can use to check interactions?
Yes. The NIAAA’s Alcohol-Medication Interaction Risk Calculator (AMIRC) is the most reliable. GoodRx and WebMD have tools too, but they’re not always updated with the latest guidelines. The best approach? Use them as a starting point, then confirm with your pharmacist. They have access to real-time databases and can tell you what’s safe for your specific situation.
If you’re taking medication and drinking alcohol, you’re not alone. But you don’t have to be at risk. A simple conversation with your pharmacist could prevent a hospital trip, a life-changing injury, or worse. Ask the question. Get the facts. Your body will thank you.