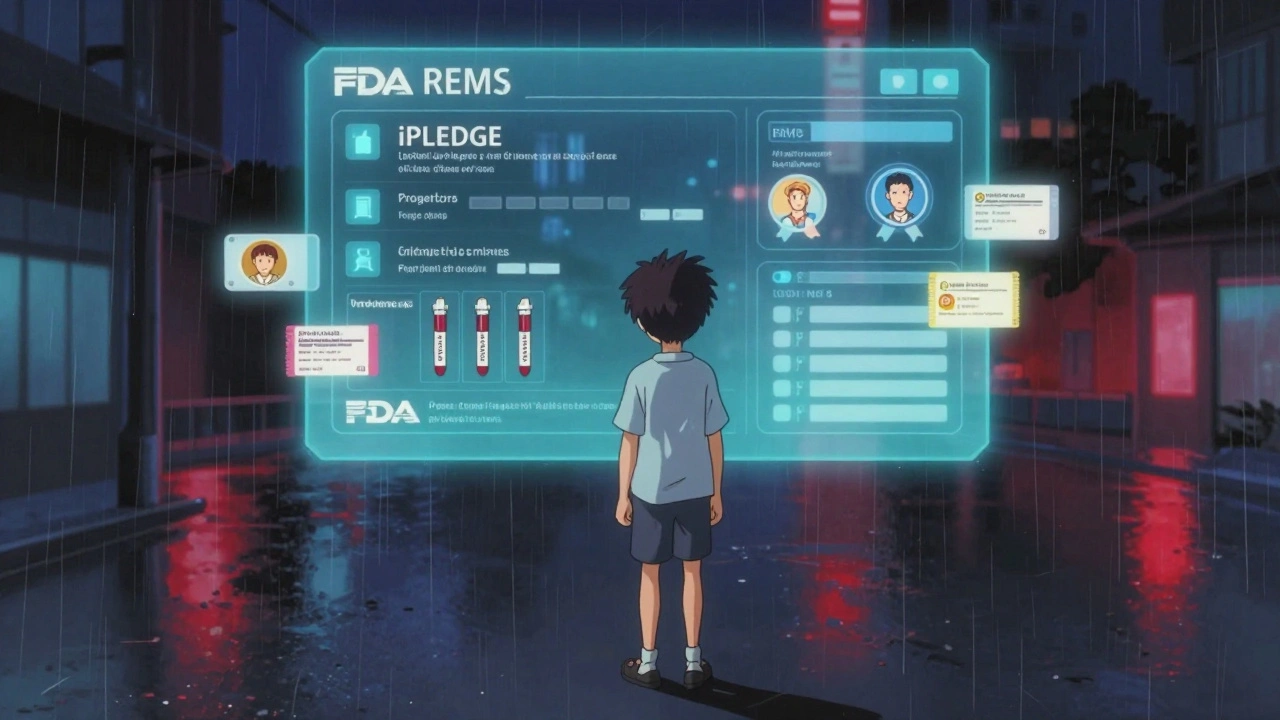
Starting a new medication isn’t just about popping a pill. If that drug has serious risks, you might be stepping into a system called REMS - Risk Evaluation and Mitigation Strategies. These aren’t optional guidelines. They’re legally required safety nets put in place by the U.S. Food and Drug Administration (FDA) to make sure the benefits of certain drugs outweigh their dangers. And if you miss checking them, your prescription could be denied, delayed, or worse - put you at risk.
What Exactly Is a REMS?
REMS are special safety programs the FDA forces drugmakers to run for medications that carry serious, sometimes life-threatening risks. Think of them as extra layers of protection. Without REMS, some drugs would never get approved because the dangers are too high. But with them, patients can still get access to treatments they need - like powerful cancer drugs, fertility medications, or opioids - while staying protected. There are 76 active REMS programs as of 2025. Some are simple. Others are complex. For example, the iPLEDGE program for isotretinoin (Accutane) requires both doctors and patients to register online before any prescription is filled. Why? Because this drug causes severe birth defects. Another one, Zyprexa Relprevv, must be injected in a certified clinic where staff watch you for at least three hours after the shot to catch rare but dangerous reactions. These aren’t just paperwork. They’re real barriers built to stop harm.How to Find Out If Your Medication Has a REMS
The first thing you or your doctor should do is check the medication’s official prescribing information. Every FDA-approved drug has this document - it’s not hidden. It’s right there in the package insert or on DailyMed, the FDA’s public database. Look for the section titled “REMS” or “Risk Evaluation and Mitigation Strategy.” If it’s there, the next step is figuring out what you need to do. You can also search the FDA’s REMS Public Dashboard. It’s free, easy to use, and updated regularly. Just type in the drug name - like “mycophenolate” or “thalidomide” - and it shows you exactly what REMS applies. The dashboard breaks it down: Is there a Medication Guide? Do prescribers need certification? Are patients required to enroll in a registry? You’ll see it all in plain language. Don’t rely on your pharmacist to know every REMS off the top of their head. They’ll check, but they’re not mind readers. Always verify yourself. Even experienced providers miss things when they’re rushed.Common REMS Requirements You Might Encounter
Not all REMS are the same. They fall into four main types:- Medication Guides: These are printed handouts you get with every fill. They explain the risks in plain language. You must receive one each time - even if you’ve taken the drug before. Many patients say they’re confusing, but they’re legally required.
- Communication Plans: These are training materials sent to doctors and pharmacists. You won’t see them, but your provider should have completed them. For example, the Opioid Analgesic REMS requires prescribers to finish continuing education on safe prescribing.
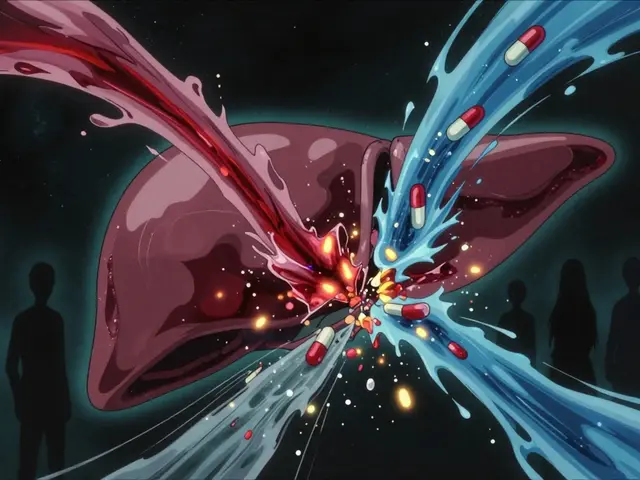
- Elements to Assure Safe Use (ETASU): This is where it gets serious. ETASU means real restrictions. You might need to:
- Register in a patient registry (like iPLEDGE)
- Get prescriber certification (like with thalidomide)
- Undergo monthly blood tests (like with clozapine)
- Only receive the drug in a certified facility (like Zyprexa Relprevv)
- Implementation Systems: These are the behind-the-scenes tools that track compliance - like electronic alerts in pharmacy systems or digital enrollment portals.
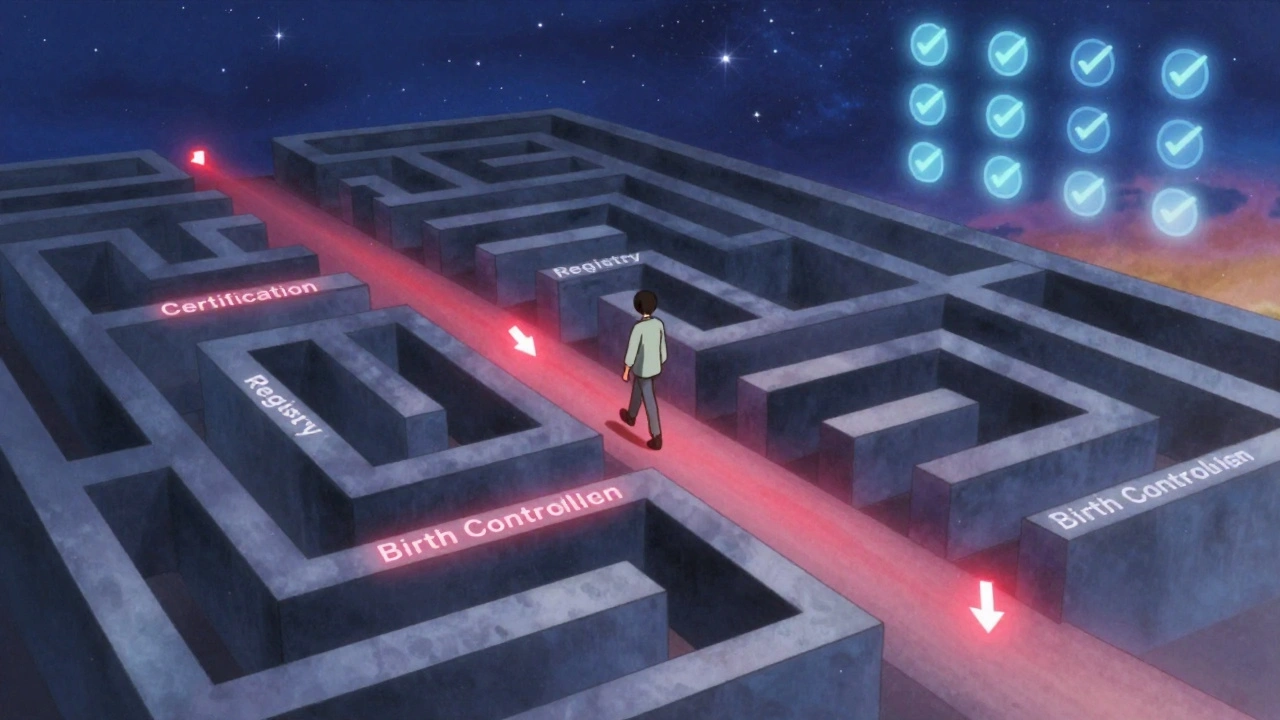
For example, if you’re prescribed mycophenolate (used after organ transplants), you’ll need to sign a form acknowledging the risk of pregnancy loss. Your doctor must be certified. And you’ll need to use two forms of birth control - with proof - for a full year before and after treatment. Miss one step? The pharmacy won’t fill it.
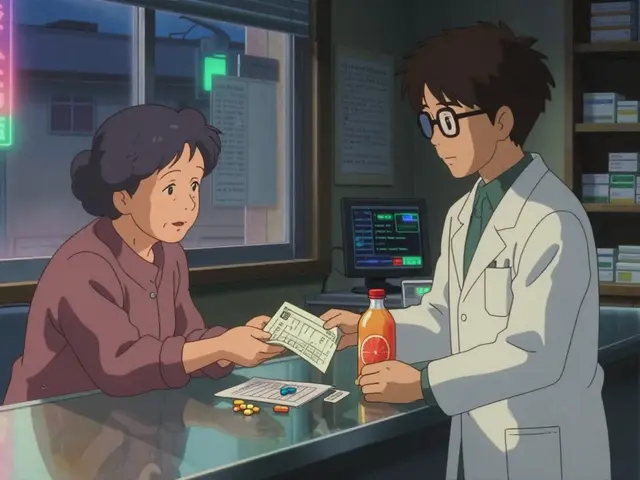
Who Does What? Roles in REMS Compliance
REMS isn’t just the doctor’s job. It’s a team effort.- Patients: You’re responsible for reading the Medication Guide, enrolling in registries if required, and telling your provider about any pregnancy plans or side effects. Don’t assume someone else is handling it.
- Prescribers: You must be certified, complete required training, and document everything. The average time to complete REMS steps per prescription? About 12.7 extra minutes, according to a 2019 AMA survey. That adds up fast.
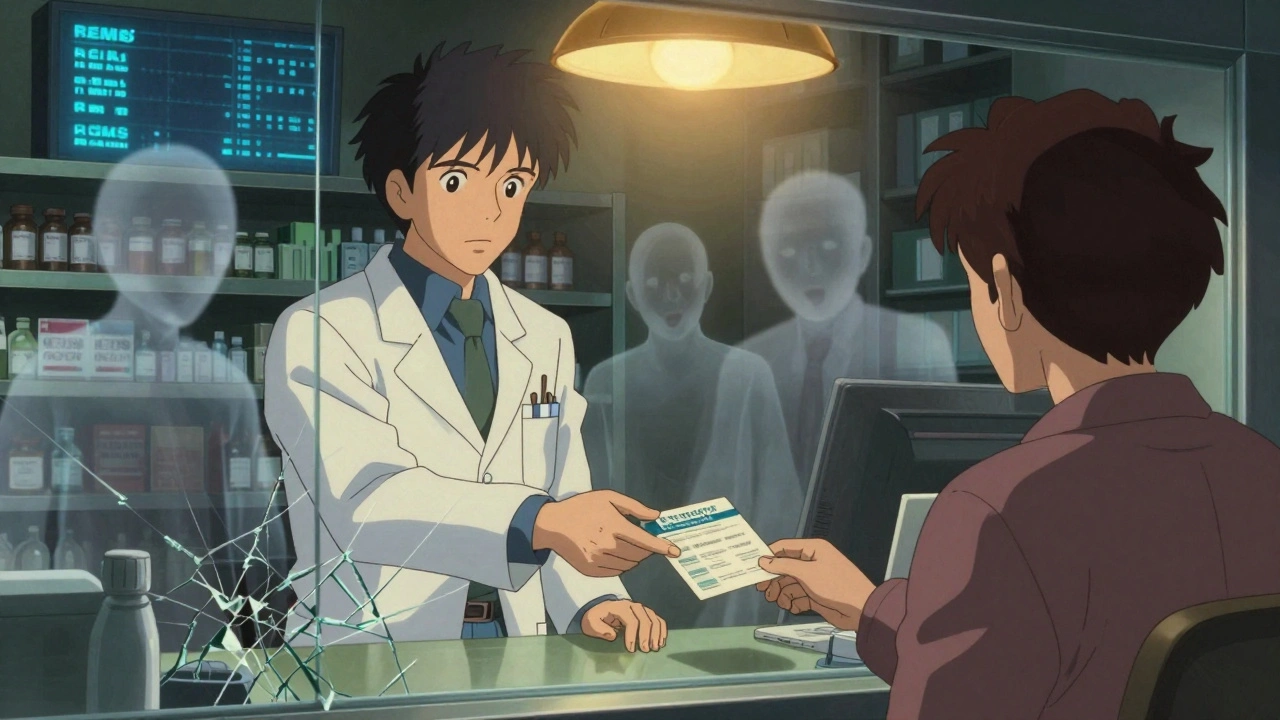
- Pharmacists: They’re the final gatekeepers. If the REMS isn’t complete, they can’t legally dispense the drug. Many pharmacies now use checklists to cut down delays. One hospital reduced isotretinoin processing from 45 minutes to 15 minutes just by standardizing their REMS verification process.
It’s not perfect. A 2022 survey by the National Organization for Rare Disorders found that 42% of patients on REMS drugs faced delays - an average of over six business days. Some people missed treatments because paperwork got lost. Others couldn’t get certified in time.
Step-by-Step: How to Verify REMS Before Starting
Follow this three-step process every time you’re prescribed a new drug:- Check the label and prescribing info. Look for the word “REMS” or “Risk Evaluation and Mitigation Strategy.” If it’s there, don’t skip ahead.
- Search the FDA REMS Public Dashboard. Go to fda.gov/drugs/risk-evaluation-and-mitigation-strategies-rems. Type in the drug name. Note all requirements: certification? registry? lab tests?
- Confirm with your pharmacy or manufacturer. Call the pharmacy that will fill your script. Ask: “Does this drug have a REMS? What do I need to do?” If they’re unsure, contact the drugmaker’s REMS website directly. For example, iPLEDGE has its own site: ipledgeprogram.com. Thalidomide’s program is at thalidomideREMS.com.
Don’t wait until the day you pick up your prescription. Start this process as soon as you get the prescription. Give yourself at least 5-7 days. Some certifications take weeks to process.
What Happens If You Skip REMS?
Skipping REMS doesn’t mean you’ll get sick right away. But it means you’re bypassing safety layers built to protect you. Pharmacies will refuse to fill the prescription. Your doctor may be fined. And if something goes wrong - like a birth defect from isotretinoin or a dangerous reaction to Zyprexa Relprevv - the legal and medical consequences can be severe. Some patients try to bypass REMS by switching doctors or pharmacies. That doesn’t work. The systems are linked. If you’re enrolled in iPLEDGE, any pharmacy can see your status. If you’re not certified, no one can legally give you the drug.Recent Changes and What’s Coming
The FDA is trying to fix the system. In 2023, they launched an updated REMS dashboard with real-time data and smartphone-friendly tools. They also started requiring all new REMS programs to include patient-facing apps. Big pharmacy benefit managers now integrate REMS checks into e-prescribing systems - meaning your doctor’s EHR might pop up a warning before the prescription even leaves the office. In 2025, the FDA is expected to finalize new rules that could cut REMS paperwork by 30-40%. But don’t expect it to disappear. Experts predict that 85-90% of new cancer drugs approved after 2025 will need REMS. The same goes for gene therapies and complex biologics. These drugs are powerful - and dangerous. The system isn’t going away. It’s just getting smarter.Final Tip: Keep Records
Save every form, email, and confirmation number related to your REMS compliance. The FDA requires providers to keep these records for at least 10 years. You should too. If you ever switch doctors, move, or need to prove you followed protocol, having those documents makes everything easier.REMS isn’t about bureaucracy. It’s about survival. For some drugs, these steps are the only reason you can get treatment at all. Do the work. Ask questions. Don’t let a missed form cost you your health.
Do all new medications have REMS requirements?
No. Only medications with serious safety risks need REMS. About 15-20% of new drugs approved by the FDA each year require a REMS. Most common medications like blood pressure pills or antibiotics do not. REMS is reserved for drugs that could cause death, birth defects, severe addiction, or life-threatening reactions.
Can I get a REMS medication without seeing my doctor in person?
It depends. For most REMS, you don’t need an in-person visit - but you do need certification. For example, the Opioid Analgesic REMS only requires doctors to complete online training. But for drugs like Zyprexa Relprevv, you must be physically present at a certified facility for the injection. Always check the specific REMS requirements for your drug.
What if I’m pregnant or planning to become pregnant?
If you’re prescribed a drug with a REMS for pregnancy risk - like isotretinoin, mycophenolate, or thalidomide - you’ll be required to use two forms of birth control and take monthly pregnancy tests. You must sign documents confirming you understand the risks. If you become pregnant while taking these drugs, stop immediately and contact your doctor. These medications can cause severe birth defects.
Why does my pharmacy keep asking me the same questions about REMS?
Because they’re legally required to verify your compliance every time. Even if you’ve taken the drug for years, they must confirm you’re still enrolled, your pregnancy tests are current, and your prescriber is certified. It’s not being difficult - it’s the law. Some pharmacies use checklists to make this faster, but the process can’t be skipped.
Are REMS programs the same in other countries?
No. REMS is a U.S.-specific system created under the FDA’s authority. Other countries have their own safety programs - like the EU’s Risk Management Plans or Canada’s Risk Evaluation and Mitigation Programs - but they’re not identical. If you’re traveling or getting medication from outside the U.S., don’t assume REMS rules apply. Always check local regulations.