What FeNO Testing Actually Measures
FeNO testing stands for Fractional Exhaled Nitric Oxide testing. It’s a simple, non-invasive way to measure how much nitric oxide is in your breath. That number tells doctors how inflamed your airways are - especially if you have asthma. Nitric oxide isn’t something you normally think about, but your body makes it naturally when there’s inflammation in your lungs. High levels mean your airways are irritated, swollen, and likely reacting to allergens or triggers. This isn’t guesswork. It’s a direct readout of type 2 inflammation, the kind that responds best to steroid inhalers.
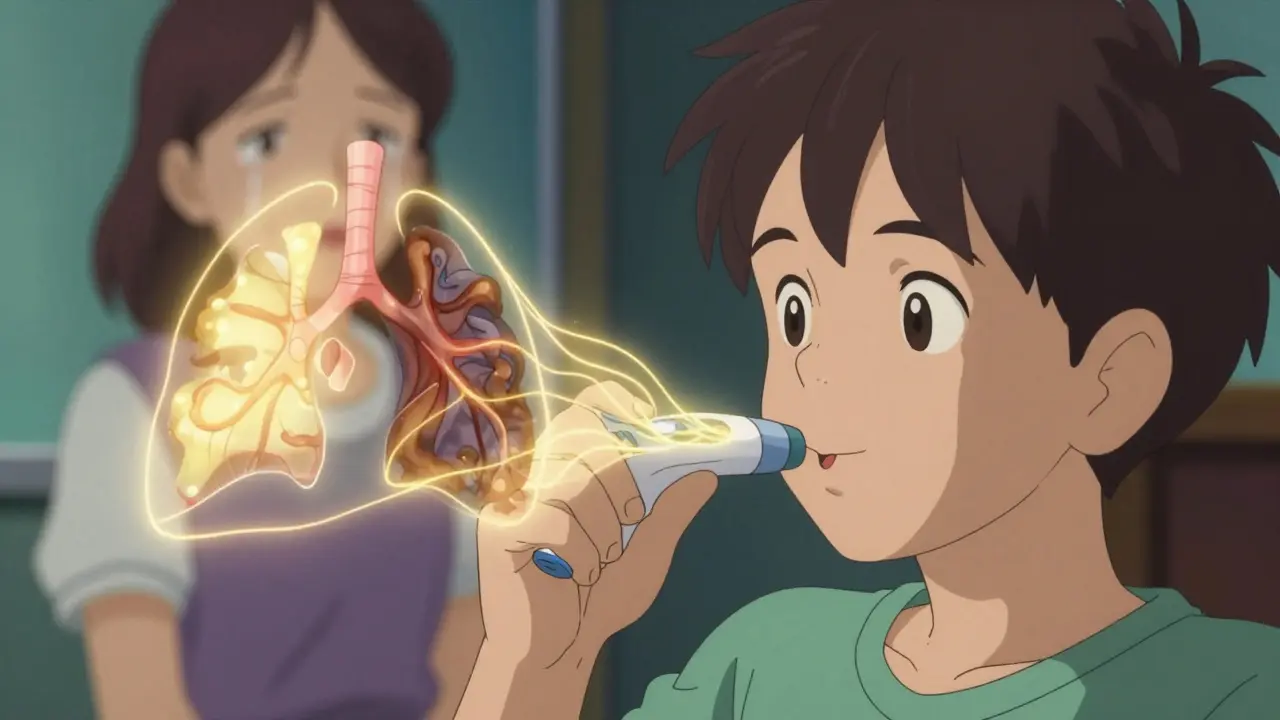
Unlike spirometry, which just tells you how well you can blow air out, FeNO shows you what’s happening inside your airways before symptoms get bad. You don’t need to do anything complicated. You breathe in deeply through a filter, then slowly exhale into a small handheld device for about 10 seconds. The machine gives you a number in parts per billion (ppb). That’s it. No needles. No blood draws. No waiting days for lab results.
Why FeNO Matters More Than You Think
Many people with asthma are told they have it because they wheeze or feel tight in the chest. But not everyone who wheezes has asthma. Some have chronic bronchitis. Others have vocal cord dysfunction. FeNO helps cut through the noise. A reading above 25 ppb in adults strongly suggests eosinophilic asthma - the type where immune cells called eosinophils are overactive and cause swelling. That’s important because it tells your doctor whether a steroid inhaler will help.
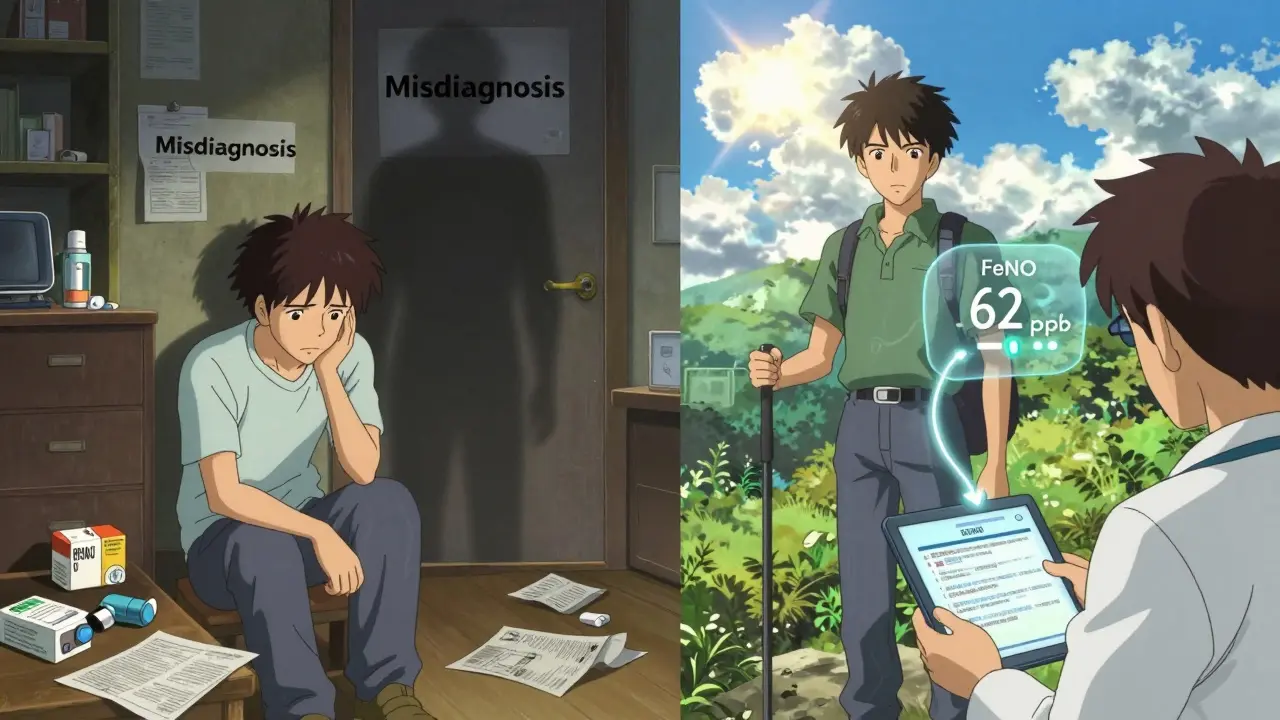
Studies show that when FeNO levels are high, asthma is up to seven times more likely than if you only rely on symptoms or lung function tests. One 2022 study found that combining FeNO with wheezing patterns and spirometry raised diagnostic accuracy to 76%. That’s a big jump. And for patients who keep having flare-ups despite using inhalers, FeNO can reveal why: their inflammation isn’t under control. In one case from the American Lung Association, a 34-year-old was misdiagnosed with bronchitis for seven years. Their FeNO level was 48 ppb - clear evidence of uncontrolled asthma.
How FeNO Compares to Other Tests
Doctors have a few tools to check for asthma inflammation. Spirometry measures airflow. Blood eosinophil counts look at immune cells in your blood. Sputum tests examine mucus under a microscope. Each has pros and cons.
- Spirometry is great for seeing how blocked your airways are, but it doesn’t tell you why they’re blocked. It’s also hard for kids, elderly patients, or anyone with severe breathing problems to do correctly.
- Blood eosinophils are easier than sputum, but they don’t always match what’s happening in your lungs. Studies show FeNO correlates better with actual airway inflammation than blood tests do.
- Sputum analysis is the gold standard for measuring lung inflammation, but it’s messy. You have to cough up mucus, and labs take days to process it. Most patients hate it.
FeNO wins on speed, comfort, and accuracy for type 2 inflammation. It’s fast, painless, and gives results in seconds. But it’s not perfect. If your asthma isn’t driven by eosinophils - like in exercise-induced or stress-triggered asthma - FeNO might be normal even if you’re struggling. That’s why it’s never used alone. It’s a piece of the puzzle, not the whole picture.
What Your FeNO Number Means
Your FeNO result is a number. But what does it mean? Here’s how doctors interpret it:
- Below 20 ppb (children) or 25 ppb (adults): Low inflammation. Your asthma is likely well-controlled, or you may not have eosinophilic asthma at all.
- 20-50 ppb (children) or 25-50 ppb (adults): Moderate inflammation. Your treatment may need adjustment. This is the gray zone where doctors look at your symptoms, inhaler use, and history.
- Above 50 ppb: High inflammation. Your airways are actively inflamed. You’re at higher risk for flare-ups, and your current meds probably aren’t enough.
These numbers aren’t magic. They’re guides. A 30-year-old who smokes might have a FeNO of 18 ppb - but that’s artificially low because smoking suppresses nitric oxide. A child with severe allergies might have a 40 ppb reading even if they feel fine. That’s why context matters. Your doctor needs to know your smoking status, recent steroid use, allergies, and how often you’re using your rescue inhaler.
Who Benefits Most From FeNO Testing?
FeNO isn’t for everyone. But it’s a game-changer for certain groups:
- People with unclear asthma diagnosis - if your symptoms are vague or overlap with other conditions.
- Patients who keep having flare-ups despite using inhalers. FeNO shows if inflammation is still high.
- Those being considered for biologic therapies - drugs like dupilumab or benralizumab only work for type 2 inflammation. FeNO helps pick the right candidates.
- Children over age five - they often can’t do spirometry well, but they can blow into a FeNO device.
- People with allergic rhinitis - since nasal allergies often go hand-in-hand with asthma, FeNO helps connect the dots.
For patients on maintenance therapy, testing every 3-4 months helps track progress. After changing meds, doctors often retest in 4-6 weeks to see if inflammation went down. One patient on Reddit said, “Finally, objective proof my inhaler wasn’t working.” That’s the power of FeNO - it takes the guesswork out of treatment.
What Can Mess Up Your FeNO Results?
FeNO is sensitive. A few things can throw off the reading:
- Smoking - cuts FeNO levels by 30-50%. If you smoke, your doctor needs to know.
- Recent steroid use - inhaled or oral steroids lower FeNO. Test before starting or changing meds.
- Eating, drinking, or exercising - avoid food, drinks (except water), and intense activity for at least an hour before testing.
- Poor technique - exhaling too fast, too slow, or with a cough can invalidate the test. Most devices give real-time feedback to help you get it right.
That’s why clinics use devices like the NIOX VERO® or NObreath®. They show you a graph as you breathe, telling you if you’re exhaling at the right speed. This cuts invalid results from 20% down to under 5%. Training for staff takes less than half an hour. It’s not complicated.
Real Stories, Real Impact
Patients who’ve had FeNO testing often say it changed their care. In a survey of 1,200 asthma patients, 68% said it improved their treatment plan. One woman in Dunedin, who’d been told her breathing issues were “just stress,” got a FeNO reading of 62 ppb. Her doctor switched her to a higher-dose steroid inhaler. Within weeks, she was back to hiking on weekends.
Another patient, a 9-year-old boy, had been on multiple inhalers for years with no improvement. His FeNO was 45 ppb. His allergist added a leukotriene modifier. His symptoms dropped by 80%. “We were going in circles,” his mom said. “FeNO finally gave us a direction.”
But it’s not perfect. Some people report inconsistent results, or their insurance won’t cover it. In the U.S., only 58% of commercial plans cover FeNO without restrictions. In the UK, it’s standard care thanks to NICE guidelines. Here in New Zealand, access is growing but still uneven. If your doctor recommends it and you’re denied, ask for a letter of medical necessity - many insurers approve it after appeal.
The Future of FeNO Testing
FeNO isn’t standing still. In early 2023, the FDA cleared the first smartphone-connected FeNO device. It’s a small mouthpiece that plugs into your phone, gives you instant results, and lets you track your levels over time. For patients on biologics, this means they can monitor inflammation at home and share data with their doctor remotely.
Researchers are also using FeNO to predict who will respond to expensive biologic drugs. If your FeNO is above 50 ppb and you have high eosinophils, you’re a strong candidate for dupilumab. That saves money and avoids trial-and-error treatment.
Studies are now underway to see if FeNO can help in rural areas where specialists are scarce. If a primary care provider can test and interpret FeNO, they can manage more asthma cases without referring every patient to a pulmonologist.
What You Should Do Next
If you have asthma and:
- Your symptoms aren’t under control
- You’re using your rescue inhaler more than twice a week
- Your doctor keeps changing your meds without clear results
- You’ve been told you have asthma but aren’t sure
Ask about FeNO testing. It’s quick, safe, and gives real data. Don’t accept vague answers like “you’re just sensitive” or “it’s all in your head.” If inflammation is driving your asthma, FeNO can prove it - and help you get the right treatment.
Bring a list of your symptoms, inhaler use, and any recent flare-ups. Ask your doctor: “Could FeNO help us understand what’s really going on?” Most will agree. And if they haven’t used it before, they can learn. The tools are simple. The science is solid. The results? Life-changing for many.
What is FeNO testing used for in asthma?
FeNO testing measures nitric oxide in your breath to detect airway inflammation, especially type 2 inflammation linked to eosinophilic asthma. It helps confirm diagnosis, predict response to steroid inhalers, and guide treatment changes to prevent flare-ups.
How accurate is FeNO testing for asthma?
FeNO has high specificity (75-95%), meaning it’s very good at confirming asthma when levels are high. But its sensitivity is lower (52-75%), so normal results don’t rule out asthma. It works best when combined with symptoms, lung function tests, and medical history.
Is FeNO testing painful or risky?
No. It’s completely non-invasive. You just breathe into a handheld device for about 10 seconds. There’s no pain, no needles, and no side effects. It’s safe for children over five and adults alike.
What should I avoid before a FeNO test?
Avoid eating, drinking (except water), smoking, and vigorous exercise for at least one hour before the test. Also, don’t use your rescue inhaler right before testing, as it can lower your FeNO reading.
Can FeNO testing replace spirometry?
No. FeNO measures inflammation; spirometry measures airflow. They do different things. FeNO tells you why your airways are tight; spirometry tells you how tight they are. Both are needed for complete asthma management.
Why might my FeNO result be normal even if I have asthma?
Not all asthma is driven by type 2 inflammation. If your asthma is triggered by exercise, cold air, or stress - and not by allergies or eosinophils - your FeNO may be normal. This is called non-eosinophilic asthma, and it doesn’t respond as well to steroids.
How often should I get FeNO tested?
For stable asthma, testing every 3-4 months is common. If you’re adjusting meds or having flare-ups, your doctor may test you every 4-6 weeks until your inflammation is under control.
Does insurance cover FeNO testing?
Coverage varies. Medicare and some private plans cover it when used for asthma management, especially if you have frequent flare-ups. In the U.S., only 58% of commercial plans cover it without restrictions. In the UK and parts of Europe, it’s standard. Always check with your provider and ask for a letter of medical necessity if denied.

