When you hear that hepatitis C has been cured, it’s natural to think the danger is over. You’ve taken the pills, cleared the virus, and your blood tests now show sustained virologic response - or SVR. That’s a win. But here’s the part no one talks about enough: SVR doesn’t mean zero risk of liver cancer. Even after the virus is gone, your liver might still be in danger.
What SVR Really Means - And What It Doesn’t
SVR means the hepatitis C virus (HCV) is undetectable in your blood 12 or 24 weeks after finishing treatment. With modern direct-acting antivirals (DAAs), over 95% of people achieve this. It’s one of the biggest medical breakthroughs in decades. Your liver can start healing. Inflammation drops. Fibrosis may even reverse.
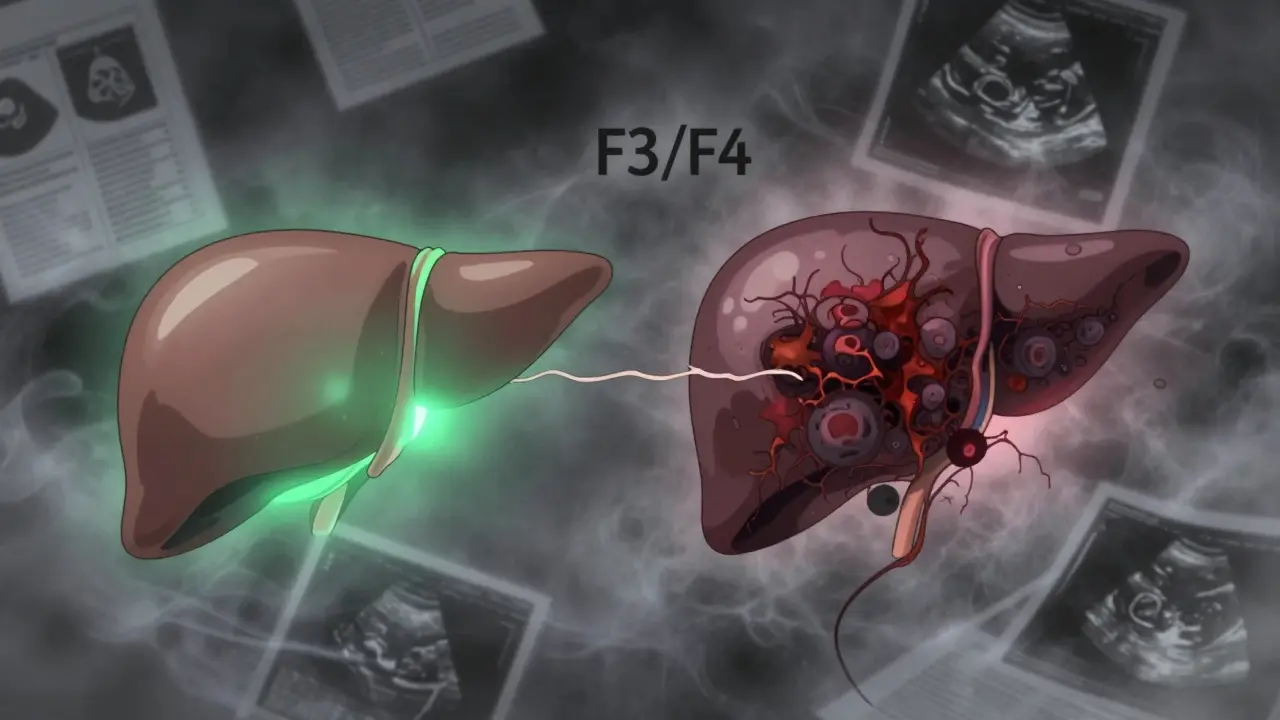
But here’s the catch: if you had advanced scarring - called fibrosis F3 or cirrhosis (F4) - before treatment, your risk of developing liver cancer doesn’t vanish. It drops by about 71%, according to a 2024 review of over 50 studies. That sounds great. But 71% isn’t 100%. You’re still at higher risk than someone who never had hepatitis C.
Think of it like quitting smoking. Your lung cancer risk plummets, but if you smoked for 20 years, your risk never goes back to that of someone who never lit up. The same logic applies to your liver.
Who Still Needs Surveillance - And Who Doesn’t
Not everyone needs ongoing liver cancer screening after SVR. The key is knowing your fibrosis stage before treatment.
- If you had no fibrosis (F0-F1) or mild fibrosis (F2): your HCC risk after SVR is extremely low. Most experts say you don’t need regular scans.
- If you had advanced fibrosis (F3): you’re in a gray zone. Some guidelines say monitor, others say don’t.
- If you had cirrhosis (F4): you absolutely need ongoing surveillance. No exceptions.
The numbers tell the story. In a 2023 JAMA study, cirrhotic patients who achieved SVR still had a liver cancer incidence rate of 2.1-2.3 per 100 person-years. That’s over 2% per year. Compare that to 4.5% in untreated cirrhotics - a big drop - but still high enough to warrant action.
And here’s what’s tricky: many people don’t know their fibrosis stage. A liver biopsy isn’t always done. That’s why tools like transient elastography (FibroScan) and the FIB-4 index are now standard. After SVR, if your FibroScan reading is above 11.2 kPa, or your FIB-4 score is over 3.25, you’re still at elevated risk - even if you were told you only had F3.
Why Guidelines Are Split - And What It Means for You
There’s a major disagreement between top liver societies.
The European Association for the Study of the Liver (EASL) says: monitor everyone with F3 or F4 after SVR. Why? Because fibrosis can be misread. Ultrasound might miss early cirrhosis. And catching liver cancer early saves lives.
The American Association for the Study of Liver Diseases (AASLD) says: only monitor those with cirrhosis (F4). They argue the risk in F3 patients is too low to justify routine scans, especially since many F3 livers improve after SVR.
This isn’t just academic. It affects real people. In the U.S., you might be told you’re fine. In Europe, you’ll get a scan every six months. Both sides have data. But the stakes are high: liver cancer caught early has a 70% survival rate. Once it spreads, that drops to under 10%.
Dr. Anna Lok, former AASLD president, stands by the U.S. position. Dr. Markus Peck-Radosavljevic, representing EASL, says: “The cost of an ultrasound is pennies compared to the cost of missing a tumor.”
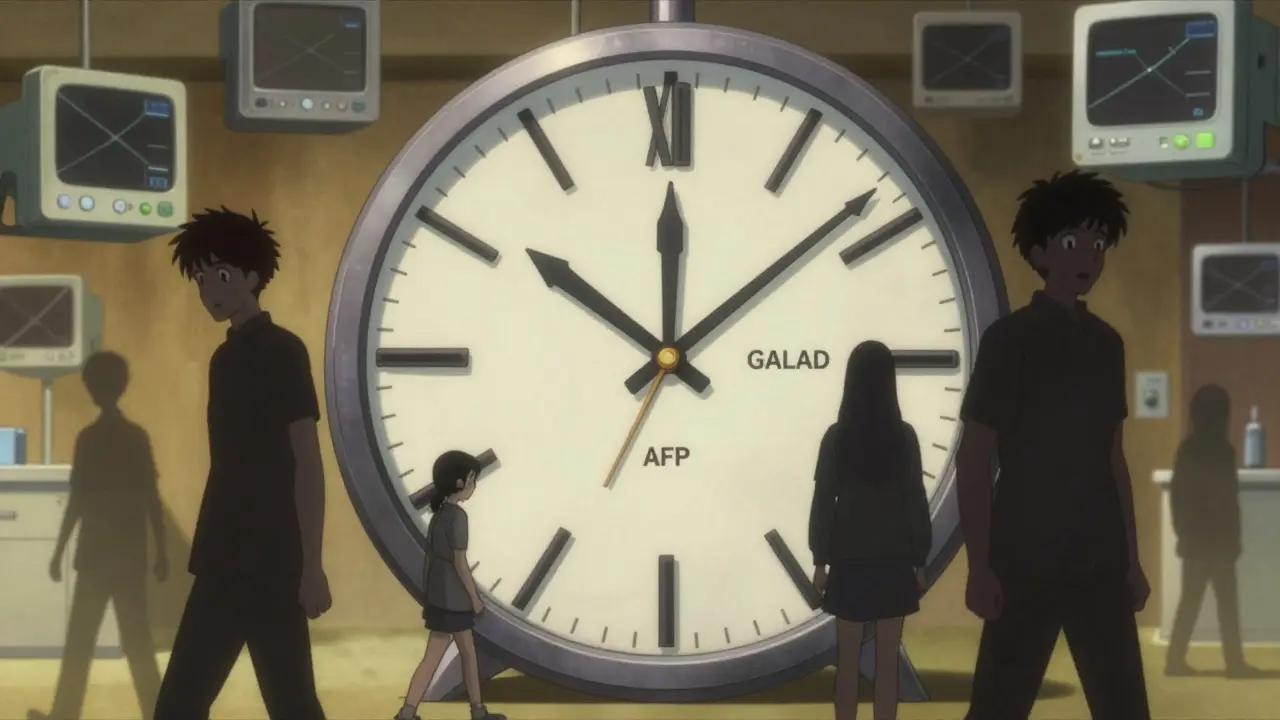
The Surveillance Routine - What You’ll Actually Do
If you’re in the high-risk group, here’s what your follow-up looks like:
- Every 6 months: abdominal ultrasound - the standard test. It’s non-invasive, cheap, and widely available.
- Often paired with: alpha-fetoprotein (AFP) blood test - though it’s not perfect. It misses up to 40% of early cancers.
- Newer options: GALAD score - a blood test combining age, gender, AFP, AFP-L3, and DCP. It’s more accurate than AFP alone and is being adopted in Europe.
Some clinics now use automated reminders. The Veterans Health Administration saw a 32% jump in screening rates after adding system alerts. If your doctor doesn’t bring it up, ask. Don’t wait.
Why So Many People Skip Screening - And How to Avoid It
Here’s the ugly truth: only about 25% of people who should be screened actually are.
Why? Because they think they’re “cured.” They feel fine. They stop seeing their doctor. They assume the virus was the only problem.
That’s dangerous. Even if your liver feels fine, cancer can grow silently. A 2024 study showed patients who achieved SVR are more likely to skip follow-ups than those still living with HCV - because they feel safe.
Don’t let that be you. Make a note: SVR = reduced risk, not zero risk. If you had cirrhosis or advanced fibrosis, your screening schedule is now part of your lifelong health plan - like getting a colonoscopy after 50.
What’s Changing - And What’s Coming
The field is evolving fast.
Researchers are testing dynamic risk models. Instead of checking every 6 months forever, your scan frequency could adjust based on how your liver heals. If your FibroScan drops below 9.5 kPa after SVR, you might only need annual scans. Early data from Massachusetts General shows this could safely reduce screening by 42% for F3 patients.
There’s also a blood test in development that looks at gene expression patterns in liver tissue. It predicted HCC risk with 92% accuracy in a 2022 Nature Medicine study. But it’s still in labs - not clinics.
Regulators are paying attention too. The FDA now acknowledges that “cure of HCV does not eliminate HCC risk in patients with advanced fibrosis.” That could change how drug labels are written and how insurers cover long-term monitoring.
And the market is growing. The global liver cancer surveillance market is expected to hit $1.8 billion by 2027. More FibroScan machines are being used worldwide. More clinics are training staff to interpret results correctly.
What You Should Do Right Now
If you’ve achieved SVR:
- Find out your fibrosis stage before treatment. Ask for your FIB-4 or FibroScan results.
- If you had F3 or F4: schedule your next ultrasound in 6 months. Don’t wait for your doctor to call.
- If you had F0-F2: you’re likely safe, but mention your history at your next check-up.
- Ask about the GALAD score - it’s becoming available in many urban clinics.
- Teach someone else. A friend, a family member. This message needs to spread.
Don’t let the success of your treatment make you careless. The virus is gone. But your liver remembers. And it’s still worth protecting.