When a limb is gone, the brain doesn’t always get the memo. Phantom limb pain isn’t in your head-it’s in your nervous system. You feel burning, stabbing, or cramping in a leg or arm that’s no longer there. It’s real. And it’s common. Around 60% to 85% of amputees experience it. For many, the pain starts within weeks of surgery. For others, it creeps in months later. What makes it worse is that doctors used to think it was all in your mind. Now we know better. Brain scans show clear activity where the missing limb used to live. This isn’t imagination. It’s neurology.
Why Phantom Limb Pain Happens
Your brain has a map of your body. Every finger, toe, and joint has a spot. When you lose a limb, that spot doesn’t just go quiet. Instead, nearby areas start taking over. A patch of brain that once handled your hand might now respond to your face or upper arm. When you touch your cheek, your brain misreads it as your missing hand being touched. That’s cortical remapping. It’s why some people feel phantom pain when they have a rash on their chest or get a hug. Nerves at the amputation site also go haywire. Damaged nerve endings form knots called neuromas. These send random signals up the spinal cord, and the brain interprets them as pain. Add in inflammation, stress, or a tight prosthetic, and the signals get louder. Weather changes? Cold or damp conditions can trigger it. Fatigue? Same thing. It’s not weakness. It’s biology.Medications: What Works and What Doesn’t
Most people start with pills. Not because they’re the best solution, but because they’re the easiest to access. The most common go-to is amitriptyline, a tricyclic antidepressant. It’s not for depression here-it’s for nerve pain. Doctors usually start with 10 mg at night. If it helps, they slowly bump it up to 50-75 mg. Side effects? Drowsiness, dry mouth, weight gain. About 60% of users report feeling sleepy, but 45% say their pain drops by half. Then there’s gabapentin and pregabalin, both anticonvulsants. Gabapentin starts at 300 mg a day, and can go up to 3,600 mg. Pregabalin starts at 75 mg, up to 600 mg. In Reddit’s amputee community, 72% of 147 users said gabapentin helped-but 58% quit because of dizziness or brain fog. That’s the trade-off. You get pain relief, but you might feel like you’re walking through syrup. Over-the-counter painkillers like ibuprofen and naproxen? They help a little at first. About 65% of users feel some relief, but for 80% of them, it fades after 3 to 6 months. They don’t touch the nerve pain. They just calm inflammation, which isn’t the real problem. For stubborn cases, doctors turn to ketamine-given through an IV. It blocks NMDA receptors, which are stuck in pain mode. Doses are low: 0.1 to 0.5 mg per kg. It’s not a daily thing. It’s a short-term reset. Some patients report pain dropping by 60% for weeks after one or two sessions. But it’s expensive, requires monitoring, and isn’t available everywhere. Opioids like oxycodone or morphine? They’re a last resort. Yes, they work. But the risk of dependence is real. The American Pain Society says to keep daily doses under 50 morphine milligram equivalents. That’s about 10-15 mg of oxycodone a day. More than that, and you’re playing Russian roulette with addiction. One study found 35% of long-term users developed dependency. That’s not worth it unless everything else has failed.Mirror Therapy: Seeing Is Believing
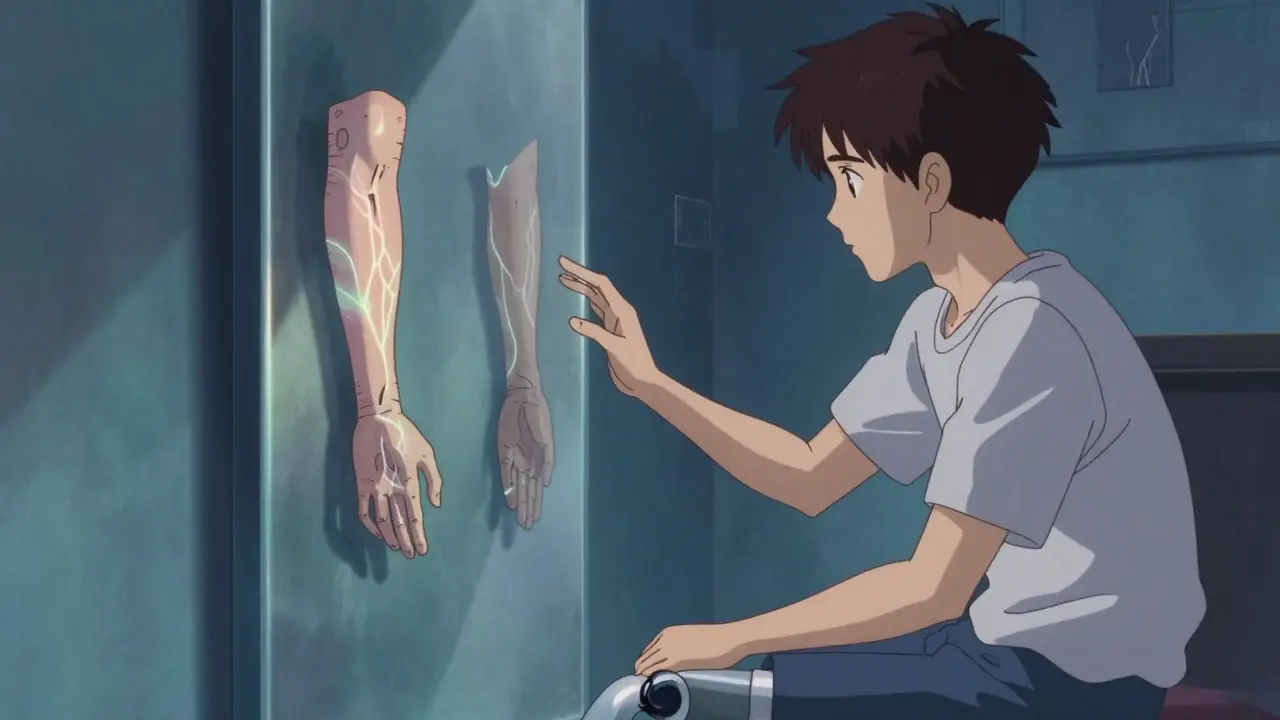
Mirror therapy is simple, cheap, and surprisingly powerful. You sit in front of a mirror, with your intact limb on one side and your stump hidden behind it. You move your good hand or foot while watching its reflection. Your brain sees two hands moving. It starts to believe the missing limb is still there-and that it’s moving without pain. This isn’t magic. It’s neuroplasticity. You’re rewiring the brain by giving it correct visual feedback. Dr. V.S. Ramachandran first proved this in the 1990s. Since then, dozens of studies show it works. In one trial, 75% of patients who did mirror therapy for 15 minutes a day, five days a week, saw pain drop by at least 50% within four weeks. But here’s the catch: you have to stick with it. About 40% of people quit within eight weeks. Why? It feels weird at first. It takes focus. You need a mirror box or even a simple mirror on a stand. You need to move slowly. You need to imagine the phantom limb moving with your real one. Some people do it while watching TV. Others do it with a therapist. The key is consistency. Ten minutes a day, every day, beats two hours once a week.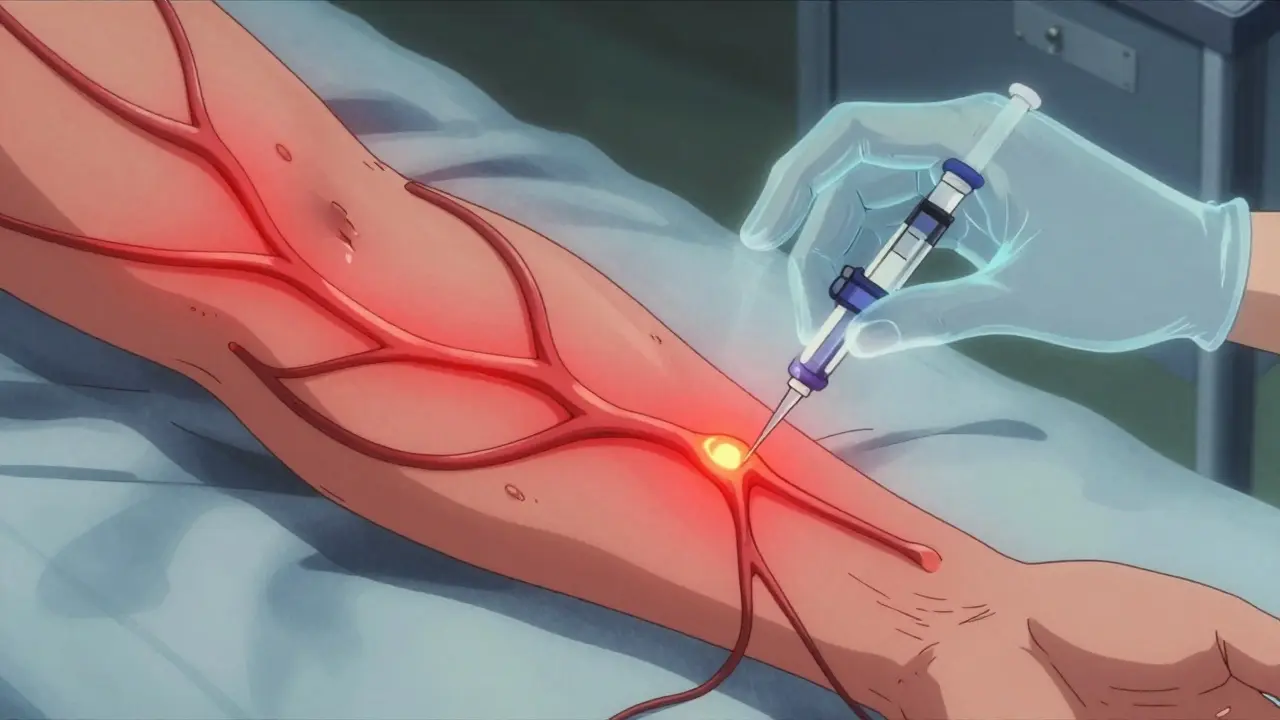
Other Non-Medication Options
If pills and mirrors aren’t enough, there are more tools. Transcutaneous Electrical Nerve Stimulation (TENS) sends tiny pulses through pads on your stump. It doesn’t fix the brain’s map, but it distracts the pain signals. Studies show 30-50% of users get relief. It’s safe, non-invasive, and FDA-cleared. You can buy a unit online, but you need to learn how to use it right-wrong settings won’t help. Botox injections into neuromas? Yes, really. A 2023 case study showed pain dropping from 8/10 to 3/10 after one injection. It lasts about 12 weeks. It’s not for everyone, but for those with localized pain from nerve knots, it’s a game-changer. Spinal cord stimulation involves implanting a device that sends electrical pulses to block pain signals. It’s surgery. It’s expensive. But for people who’ve tried everything else, it works for 40-60% of them. The FDA approved a new smart version in January 2024-Saluda Medical’s Evoke-that adjusts automatically based on your movement. Early results show 65% average pain reduction. Biofeedback teaches you to control your body’s responses. You watch your muscle tension or skin temperature on a screen and learn to relax. It’s slow. It takes weeks. But 25-40% of users see lasting improvement. It’s good for people who want to reduce stress-triggered flare-ups.What Doesn’t Work (And Why)
Some treatments sound promising but fall flat. Epidural anesthesia during surgery was once thought to prevent phantom pain. Turns out, it doesn’t. Studies show no clear benefit. Herbal supplements? No solid evidence. CBD oil? Some people swear by it, but no large trials prove it works for phantom pain. Acupuncture? Might help with general relaxation, but not the root cause. And don’t expect a single pill to fix everything. The truth? Phantom limb pain has multiple causes: nerve damage, brain rewiring, inflammation, stress. So one treatment won’t cut it. You need a combo.Putting It All Together: A Realistic Plan
If you’re dealing with phantom limb pain, here’s what actually works in real life:- Start with low-dose amitriptyline or gabapentin. Give it 4-6 weeks. Track your pain on a scale of 1-10.
- Add mirror therapy. Do it daily. Use a mirror box. Move slowly. Watch the reflection. Don’t skip days.
- If pain flares with stress, try biofeedback or mindfulness. Breathe. Relax your shoulders. Your nervous system is on high alert.
- If you have a neuroma, ask about Botox. It’s quick, local, and often effective.
- If nothing’s working after 3 months, talk to a pain specialist about spinal cord stimulation or ketamine.

What’s Coming Next
The future of phantom pain treatment is getting smarter. Virtual reality mirror therapy is already in trials. Instead of a mirror, you wear a headset and see a digital limb that moves with your real one. Early results suggest it boosts adherence-people stick with it longer because it feels more immersive. New drugs are in the works too. Targeted NMDA blockers that work like ketamine but without the side effects. One Phase II trial showed 50% pain reduction at half the dose. That could be a game-changer by 2027. And hospitals? More of them are setting up specialized pain clinics. These teams include neurologists, physical therapists, psychologists, and pain specialists-all working together. That’s the gold standard now. Not one pill. Not one trick. A plan built for you.Frequently Asked Questions
Is phantom limb pain real or just in my head?
It’s real-and it’s physical. Brain scans show activity in areas that once controlled the missing limb. This isn’t psychological. It’s neurological. The brain rewires itself after amputation, and those changes cause real pain signals. It’s not weakness, imagination, or depression. It’s your nervous system adapting in a way that backfires.
How long does phantom limb pain last?
For some, it fades within weeks or months. But if it lasts more than six months, the chance of it disappearing on its own is extremely low. That’s why early treatment matters. Waiting too long makes the brain’s pain pathways stronger and harder to reverse. Don’t assume it’ll go away. Take action early.
Can mirror therapy really help, or is it just a gimmick?
It’s not a gimmick. Mirror therapy is backed by decades of research. It works by tricking the brain into seeing movement where there’s none, helping it unlearn pain signals. Studies show 75% of patients who stick with it for four weeks see at least a 50% drop in pain. The problem isn’t the therapy-it’s sticking with it. Most people quit too soon because it feels strange at first.
Why do some medications stop working over time?
Your body can build tolerance, especially to drugs like gabapentin or opioids. Also, phantom pain isn’t static. As your brain rewires further, the pain changes. What worked at first might not work six months later. That’s why treatment needs to be flexible. You might start with amitriptyline, then add mirror therapy, then try TENS. It’s a process, not a one-time fix.
Are there any risks with mirror therapy?
No major risks. It’s safe, non-invasive, and drug-free. Some people feel dizzy or disoriented at first, especially if they’re not used to visual tricks. That usually passes quickly. If you have severe vertigo or epilepsy, talk to your doctor first-but for most people, it’s as safe as stretching.
Should I avoid opioids completely?
Not necessarily-but use them only as a last resort. Opioids can help with severe pain in the short term, but the risk of dependence is high. The American Pain Society recommends keeping daily doses under 50 morphine milligram equivalents. If you’re on opioids for more than a few weeks, you need regular monitoring. Many people end up worse off after long-term use. Try everything else first.