Hypertension Medication Selector
Quick Snapshot
- Accupril (quinapril) is an ACE inhibitor that relaxes blood vessels.
- Biggest alternatives fall into three classes: ACE inhibitors, ARBs, calcium‑channel blockers, and thiazide diuretics.
- Key decision factors include side‑effect profile, kidney function, and cost.
- Switching drugs requires a 1‑week washout for most ACE inhibitors.
- Combining a low‑dose ACE inhibitor with a diuretic often yields the best BP control.
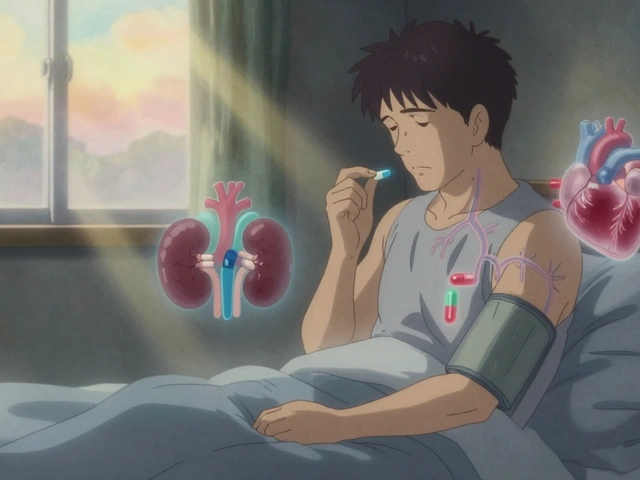
Accupril is a brand‑name ACE inhibitor whose generic name is quinapril, prescribed to lower high blood pressure and reduce strain on the heart.
How Accupril Lowers Blood Pressure
Accupril blocks the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor. By curbing this hormone, blood vessels stay relaxed, allowing blood to flow more easily. The drug also modestly lowers aldosterone, reducing sodium retention and further easing pressure on the arterial walls.
Typical starting dose for adults is 10‑20mg once daily, adjusted up to 40mg based on response and kidney function. Because it’s excreted partly through the kidneys, doctors monitor creatinine and potassium levels regularly.
Major Alternatives on the Market
When doctors consider a switch or add‑on therapy, they look at four main drug families. Below are the most frequently prescribed members.
Lisinopril is another ACE inhibitor that shares the same mechanism as Accupril but tends to have a simpler dosing schedule (once daily up to 40mg).
Losartan is an angiotensinII receptor blocker (ARB). It blocks the same hormone downstream, making it a good choice for patients who develop cough on ACE inhibitors.
Amlodipine belongs to the calcium‑channel blocker (CCB) class. It relaxes the smooth muscle in arterial walls and works well when blood pressure spikes in the evenings.
Hydrochlorothiazide is a thiazide diuretic that helps the kidneys excrete excess salt and water, lowering volume‑related pressure.
Each of these drugs carries its own pros and cons, which we’ll unpack in the comparison table.
| Drug (Brand) | Generic Name | Class | Typical Daily Dose | Common Side Effects | Notable Advantages |
|---|---|---|---|---|---|
| Accupril | Quinapril | ACE inhibitor | 10‑40mg | Cough, elevated potassium, rare angio‑edema | Strong evidence for heart‑failure benefit |
| Prinivil | Lisinopril | ACE inhibitor | 10‑40mg | Cough, dizziness | Once‑daily dosing, cheap generic |
| Cozaar | Losartan | ARB | 25‑100mg | Elevated potassium, rare renal impairment | Less cough, safe in diabetics |
| Norvasc | Amlodipine | Calcium‑channel blocker | 5‑10mg | Swelling (edema), flushing | Effective for isolated systolic hypertension |
| Microzide | Hydrochlorothiazide | Thiazide diuretic | 12.5‑25mg | Low potassium, increased urination | Strong volume‑reduction, inexpensive |

Choosing the Right Agent: Decision Criteria
Doctors weigh four core factors when deciding between Accupril and its rivals:
- Side‑effect tolerance: A persistent dry cough points toward an ARB such as Losartan.
- Kidney function: ACE inhibitors and ARBs both affect glomerular filtration; if eGFR <30ml/min, a CCB like Amlodipine may be safer.
- Cost & insurance coverage: Generic lisinopril and hydrochlorothiazide often cost under $5 per month, while branded Accupril may be pricier.
- Comorbidity profile: Patients with heart failure gain extra mortality benefit from ACE inhibitors (Accupril, lisinopril) compared with diuretics alone.
In practice, many clinicians start with a low‑dose ACE inhibitor, add a thiazide diuretic if BP stays above target, and switch to an ARB only if cough emerges. This stepwise approach aligns with American Heart Association guidelines and FDA prescribing information.
Practical Tips for Switching or Combining Therapies
- Washout period: When moving from one ACE inhibitor to another, a 24‑hour gap is enough; from ACE inhibitor to ARB, a 48‑hour gap reduces angio‑edema risk.
- Start low, go slow: Begin any new antihypertensive at the lowest approved dose and titrate every 2‑4 weeks while checking blood pressure and electrolytes.
- Monitor potassium: ACE inhibitors and ARBs can raise potassium; if >5.0mmol/L, add a low‑dose thiazide or adjust diet.
- Watch for drug interactions: NSAIDs blunt the effect of ACE inhibitors and can worsen kidney function; advise patients to limit ibuprofen use.
- Educate on symptom tracking: Encourage patients to log any new cough, swelling, or dizziness and report within a week.
Related Concepts and Next Steps
Understanding Accupril’s place in hypertension management opens doors to several adjacent topics:
- Impact of lifestyle changes (diet, exercise, stress reduction) on medication dose requirements.
- Role of ambulatory blood‑pressure monitoring for true treatment efficacy.
- Long‑term renal protection strategies when using ACE inhibitors or ARBs.
- Guidelines for combination therapy in resistant hypertension.
Readers who want to dive deeper might explore "ACE inhibitor‑induced cough mechanisms" or "Choosing a first‑line antihypertensive for diabetic patients" as natural follow‑up reads.
Frequently Asked Questions
What makes Accupril different from other ACE inhibitors?
Accupril (quinapril) has a slightly longer half‑life than lisinopril, allowing once‑daily dosing with a modest once‑daily peak effect. Clinical trials cited by the FDA also highlight a stronger reduction in left‑ventricular remodeling, making it a preferred choice for patients with early heart‑failure signs.
Can I take Accupril with a diuretic like hydrochlorothiazide?
Yes. Combining an ACE inhibitor with a thiazide diuretic is a common strategy that often lowers systolic pressure by an extra 5‑10mmHg. Doctors typically start hydrochlorothiazide at 12.5mg and watch potassium levels, adjusting as needed.
Why do some patients develop a cough on Accupril?
ACE inhibitors block the breakdown of bradykinin, a peptide that can irritate the airway lining. About 5‑10% of users report a dry, persistent cough. If it becomes bothersome, switching to an ARB like Losartan usually resolves the symptom.
Is Accupril safe during pregnancy?
No. ACE inhibitors are classified as pregnancy‑category D because they can cause fetal renal dysfunction and skull ossification defects, especially in the second and third trimesters. Women of child‑bearing age should be switched to a methyldopa or labetalol regimen if pregnancy is planned.
How quickly does Accupril start lowering blood pressure?
Blood‑pressure reduction can be observed within 2‑4hours of the first dose, with maximal effect typically reached after 2‑3weeks of consistent therapy.
What monitoring is required while on Accupril?
Baseline labs should include serum creatinine, eGFR, and potassium. Repeat testing is recommended 1‑2weeks after initiation and then every 3‑6months, or sooner if symptoms arise.
Can Accupril be taken with other blood‑pressure drugs?
Yes, it can be part of a multi‑drug regimen. The most common combinations are ACE inhibitor+thiazide diuretic or ACE inhibitor+calcium‑channel blocker. However, avoid combining two drugs that both raise potassium (e.g., ACE inhibitor+spironolactone) without close lab monitoring.