Ever eaten a big meal and felt like your stomach is staging a rebellion? Bloating, gas, cramps, or fatty stools that just won’t quit? You’re not alone. Millions of people turn to digestive enzyme supplements hoping for relief. But here’s the truth: digestive enzymes aren’t a magic fix for every stomach issue. They work wonders for some - and do nothing, or even make things worse, for others.
What Digestive Enzymes Actually Do
Your body makes enzymes naturally - mostly in the pancreas - to break down food. Amylase handles carbs, protease breaks down proteins, and lipase digests fats. A healthy pancreas pumps out 800-1,500 mL of pancreatic juice every day. That’s enough to process everything you eat without a second thought. But when that system breaks down, things go sideways. If your pancreas isn’t producing enough enzymes - a condition called exocrine pancreatic insufficiency (EPI) - you can’t absorb nutrients properly. Fat slips through undigested, leading to oily, foul-smelling stools. You might lose weight, feel tired, or develop vitamin deficiencies. EPI affects 1-5% of the general population, but up to 90% of people with pancreatic cancer or chronic pancreatitis have it. That’s where prescription digestive enzyme supplements come in. Products like Creon, Zenpep, and Pancreaze are FDA-approved drugs. They’re made from pig pancreas tissue and come in enteric-coated capsules that survive stomach acid. Each capsule contains precise amounts of lipase, protease, and amylase - often 10,000 to 40,000 lipase units per dose. These aren’t supplements. They’re medical treatments.When OTC Enzymes Might Help (And When They Won’t)
Over-the-counter (OTC) enzyme supplements are a different story. They’re sold as dietary supplements, not medicines. That means they don’t have to prove they work before hitting shelves. Most contain enzymes from microbes like Aspergillus oryzae or Rhizopus arrhizus, which work in a wider pH range than animal-based enzymes. But they often lack enteric coating, meaning stomach acid can destroy them before they do any good. A 2019 analysis found OTC enzyme products vary by 20-30% in enzyme content from batch to batch. ConsumerLab tests showed 15-25% of them contain less than 80% of what’s listed on the label. So even if you buy a bottle labeled “20,000 lipase units,” you might be getting only 15,000 - or less. So who benefits? For people with lactose intolerance, lactase enzyme supplements like Lactaid work well. About 82% of users report being able to eat dairy without symptoms. For those with IBS or trouble digesting beans, broccoli, or onions, OTC enzymes like Digestive Gold (Enzymedica) can reduce bloating and gas in 50-60% of cases. Dr. Russell Havranek, a gastroenterologist with 15 years of clinical experience, says he often recommends these for IBS patients - not because they cure anything, but because they ease symptoms. But here’s the catch: if you have EPI, OTC enzymes won’t cut it. Prescription PERT reduces fatty stools by 70-85%. OTC versions? Only 30-40%. That’s not a placebo effect - it’s science. If you’re losing weight, having oily stools, or feeling constantly drained, you need real medical treatment, not a bottle from the supplement aisle.How to Take Them Right
Timing matters more than you think. Enzymes need to be in your gut when food arrives. Take them within 15 minutes before eating. If you wait until halfway through your meal, they’re already too late. For slow eaters, splitting the dose - half before, half halfway through - can improve results by 35%, according to a 2018 trial. Dosage isn’t one-size-fits-all. Start low: 10,000 lipase units per meal. Wait a week. If bloating or gas persists, bump it up by 10,000 units. Most people find their sweet spot between 25,000 and 50,000 units per meal. Severe EPI might need up to 75,000. But never go above 80,000 without a doctor’s guidance. Fat content matters too. One gram of fat needs about 500 lipase units to digest properly. A burger with 30g of fat? That’s 15,000 units right there. A salad with 5g? Maybe 2,500. Adjust accordingly.
The Hidden Risks
Enzymes aren’t risk-free. Taking them with proton pump inhibitors (PPIs) like omeprazole can backfire. PPIs lower stomach acid, which is needed to activate some enzymes. That’s why some people on PPIs say enzymes “don’t work” - they’re being neutralized before they even start. There’s also the risk of bezoars - hard lumps of undigested food - especially if you take too little enzyme for a high-fat meal. It’s rare (about 0.5% of users), but it happens. And here’s a big one: if you have SIBO (small intestinal bacterial overgrowth), enzymes can make bloating worse. Why? They feed the bad bacteria by breaking down carbs faster, giving them more fuel to ferment. If you’ve tried enzymes and got worse, get tested for SIBO before trying again.Prescription vs. OTC: The Real Difference
| Feature | Prescription PERT (Creon, Zenpep) | OTC Supplements (NOW Foods, Digestive Gold) |
|---|---|---|
| Regulation | FDA-approved drug | Dietary supplement (DSHEA) |
| Enzyme Source | Porcine (pig pancreas) | Microbial (fungi/bacteria) |
| Enteric Coating | Yes - survives stomach acid | Usually no |
| Dose Consistency | High - exact units per capsule | Low - 20-30% variation between batches |
| Efficacy for EPI | 70-85% | 30-40% |
| Efficacy for IBS/Lactose | Effective, but overkill | 50-60% |
| Cost per Dose | $1.50-$3.00 (with insurance) | $0.50-$1.00 |
| Insurance Coverage | 70-90% covered (Medicare Part D) | None |
What Experts Say
The American Gastroenterological Association says PERT is a “strongly recommended” treatment for EPI - that’s their highest level of evidence. But for IBS, functional dyspepsia, or “leaky gut”? They say there’s “insufficient evidence.” Dr. Shane from the University of Miami puts it bluntly: “OTC supplements aren’t designed to treat GI ailments.” And Dr. Levinson points out that 78% of marketing claims - especially for weight loss or “systemic health benefits” - have no clinical backing. The FDA issued 12 warning letters to enzyme supplement makers in 2022 for false claims. But Dr. Schneider from Cleveland Clinic acknowledges that some studies show enzymes help reduce symptoms. The problem? Most trials are small. More large-scale research is needed.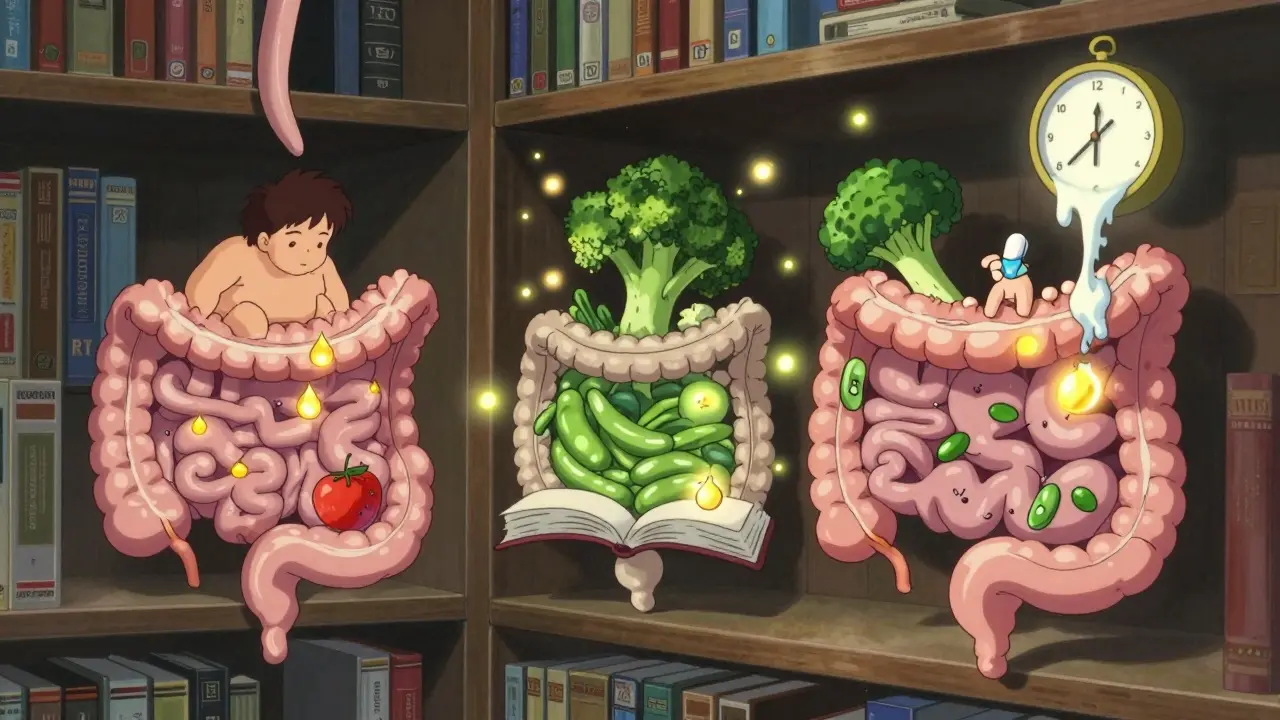
Real People, Real Results
On Reddit, users with EPI say PERT changed their lives. One wrote: “I went from 120 lbs to 170 lbs in six months. No more oily stools. I can eat cheese again.” In contrast, IBS sufferers on r/IBS report mixed results. “Digestive Gold helped with bloating after pasta, but not after beans,” says one user. Another: “I tried three brands. None worked. Stopped after a month.” A 2022 survey found 41% of IBS patients quit enzyme supplements within three months because they didn’t help. But 78% of EPI patients stick with PERT long-term. And lactase? That’s the outlier. Lactaid has over 8,000 reviews on Target.com. 82% say it lets them eat dairy without pain. Simple. Proven. Effective.What to Do Next
If you’re having persistent GI symptoms - bloating, diarrhea, weight loss, fatty stools - don’t guess. See a doctor. Get tested for EPI, SIBO, celiac disease, or other conditions. Enzymes won’t fix the root cause. If you have EPI: get a prescription. Don’t rely on OTC. It’s not worth the risk. If you have IBS or lactose intolerance: try an OTC enzyme with lactase or broad-spectrum enzymes. Start low. Track your symptoms. If nothing changes in two weeks, stop. There are better options. If you’re taking PPIs: talk to your doctor before starting enzymes. You might need to adjust timing or dosage. And skip the hype. No enzyme supplement will “boost your metabolism,” “detox your gut,” or “cure leaky gut.” Those are marketing words, not science.What’s Next in Enzyme Therapy
Research is moving fast. Scientists are engineering enzymes that work in even lower pH levels (down to 2.5), making them more reliable. One new combo - lactase plus Bifidobacterium - reduced symptoms 45% better than lactase alone in a 2023 trial. Startups like Viome are testing your gut microbiome and recommending personalized enzyme blends. It’s early, but it’s promising. For now, stick with what works: prescription enzymes for EPI, lactase for lactose intolerance, and a good doctor for everything else.Can digestive enzymes help with IBS?
Yes, for some people. OTC broad-spectrum enzymes can reduce bloating, gas, and diarrhea in 50-60% of IBS patients, especially after high-FODMAP meals. But they don’t cure IBS. If you don’t feel better after two weeks, stop. Other treatments like low-FODMAP diets or peppermint oil may work better.
Are OTC digestive enzymes safe?
Generally yes, if used as directed. But they’re not regulated like drugs. Many contain less enzyme than labeled. Some can worsen symptoms if you have SIBO. Avoid if you have acute pancreatitis. Always check with your doctor if you’re on other meds, especially PPIs.
Do I need a prescription for digestive enzymes?
Only if you have exocrine pancreatic insufficiency (EPI). That’s when your pancreas can’t make enough enzymes. Prescription PERT (like Creon) is the only effective treatment. For lactose intolerance or occasional bloating, OTC enzymes are fine - no prescription needed.
How long does it take for digestive enzymes to work?
If they’re going to work, you’ll notice within a few meals - usually 1-3 days. For EPI, relief from fatty stools and bloating can be dramatic within a week. For IBS, it’s more subtle. If you don’t see improvement after 10-14 days, the supplement likely isn’t helping you.
Can digestive enzymes cause constipation?
Yes, especially with prescription PERT. About 27% of users report constipation as a side effect. This happens when fat is digested too efficiently, reducing stool volume. If you get constipated, try increasing fiber or fluids. If it persists, talk to your doctor about adjusting your dose.
Is it okay to take digestive enzymes every day?
If you have EPI, yes - you’ll need them with every meal for life. For IBS or lactose intolerance, daily use is fine if it helps. But don’t take them long-term without knowing why. If your symptoms improve, try going off them for a few weeks to see if you still need them.