Ever looked in the mirror and noticed dark patches on your cheeks, forehead, or upper lip? You’re not alone. Many people assume these spots are just sun damage-but they might actually be melasma, a very different-and far more stubborn-condition. The truth is, treating melasma like a sunspot can make it worse. And if you’re using the wrong cream or skipping sunscreen, you’re wasting time and money.
What’s Really Causing Your Dark Patches?
Hyperpigmentation means your skin is making too much melanin in certain spots. But not all dark spots are created equal. Two of the most common types are melasma and solar lentigines (sun damage). They look similar, but their causes, behavior, and treatment needs are completely different. Melasma shows up as large, blurry, symmetrical patches-usually on the face. It’s most common in women with medium to dark skin tones (Fitzpatrick types III-VI). Hormones play a big role: pregnancy, birth control pills, and hormone replacement therapy can trigger it. Even visible light from windows or screens can make it worse. Studies show visible light contributes to 25-30% of melasma cases, which is why regular sunscreen isn’t enough. Sun damage, on the other hand, shows up as small, well-defined brown spots-often called liver spots or age spots. These appear on areas that get the most sun: face, hands, shoulders. They’re caused by years of UV exposure. Almost 90% of fair-skinned people over 60 have them. Unlike melasma, they don’t flare up with hormones or indoor light. They’re purely a result of cumulative sun exposure.Why Melasma Won’t Go Away Like Sun Spots
Here’s the catch: melasma doesn’t respond well to lasers or light treatments that work great on sun spots. Why? Because melasma is triggered by heat and light. Treatments like IPL (Intense Pulsed Light) can actually make melasma darker by stimulating melanocytes-the cells that make pigment. Studies show a 30-40% risk of worsening melasma after IPL, while sun spots usually clear up in 1-2 sessions. Melasma is also far more likely to come back. Even after noticeable improvement, over 80% of people see it return within a year if they stop being strict about sun protection. The Mayo Clinic reports that melasma improves by only 40-60% in six months with treatment, while sun damage improves by 75-90% in just 2-3 months. And here’s something many don’t realize: melasma affects Black, Asian, and Hispanic women 3-5 times more often than Caucasian women. Hormonal triggers account for 60-70% of cases in women of reproductive age. That’s why it’s not just a ‘cosmetic’ issue-it’s tied to biology, lifestyle, and environment.The Topical Agents That Actually Work
If you’re using an over-the-counter brightening cream and nothing’s changed after three months, you’re not alone. Most don’t contain enough active ingredients. Real results come from prescription-grade topicals used correctly. Hydroquinone (4%) is still the gold standard. It blocks tyrosinase, the enzyme that makes melanin. But it’s not a magic bullet. Used alone, it helps about 30-40% of people. Used in a triple combination with tretinoin and a corticosteroid, effectiveness jumps to 50-70%. This combo is now the first-line treatment for moderate melasma-up from 45% of dermatologists using it in 2018 to 75% today. But you can’t use it forever. Limit use to 3 months at a time to avoid a rare side effect called ochronosis, where skin turns darker instead of lighter. Tretinoin (0.025-0.1%) doesn’t lighten pigment directly. Instead, it speeds up skin cell turnover, helping shed the darker cells faster. It’s often paired with hydroquinone. But it can cause redness and peeling, especially at first. Start slow: use it every other night, then build up. Vitamin C (L-ascorbic acid) at 10-20% works as an antioxidant. It reduces existing melanin and blocks new production. It’s gentle, safe for daily use, and works well with sunscreen. Many dermatologists recommend applying it in the morning before sunscreen. Newer options are gaining ground. Tranexamic acid (5% topical) showed 45% improvement in melasma in a 12-week study with no major side effects. Cysteamine cream (10%) had 60% improvement in clinical trials. Both are promising, especially for people who can’t tolerate hydroquinone.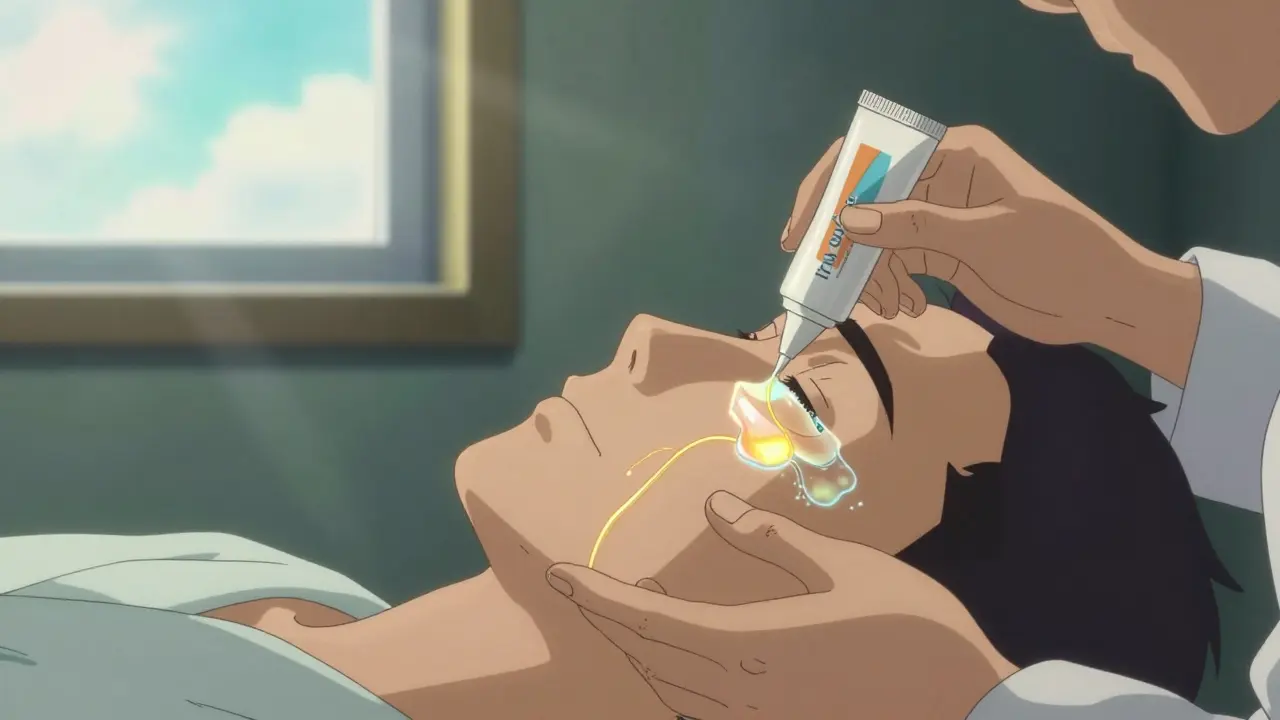
Sun Protection: The Only Non-Negotiable
No cream, no laser, no treatment will work if you’re not protecting your skin every single day. And not just UV protection. Standard sunscreens block UV rays-but melasma is also triggered by visible light and infrared heat. That’s why mineral sunscreens with iron oxides are essential. Iron oxides block visible light. Look for sunscreens labeled “broad spectrum SPF 50+” with zinc oxide and iron oxides. Apply at least a quarter-teaspoon to your face. Reapply every two hours if you’re outside-even on cloudy days. And yes, even indoors. Visible light passes through windows. If you sit near a sunny window all day, your melasma can worsen. Dermatologists now recommend daily sunscreen even if you’re working from home. The biggest mistake? Under-applying sunscreen. YES Medspa’s data shows 70% of patients use less than half the recommended amount. That’s like wearing a raincoat with three buttons fastened.Combining Treatments for Better Results
Topical treatments alone work-but they work better with professional help. Chemical peels (glycolic or salicylic acid) done every 4-6 weeks can boost results by 35-50%. But they’re risky for darker skin tones (Fitzpatrick IV-VI), who make up 40% of hyperpigmentation cases. If done too often or too deeply, they can cause post-inflammatory hyperpigmentation (PIH), which is even harder to treat. Laser treatments? Only after melasma is under control. Dermatologists now use a “melanocyte rest” protocol: 8-12 weeks of topical suppression before any laser. This drops recurrence rates from 60% to 25%. For sun damage, lasers can be used right away. For melasma? Patience is everything.

