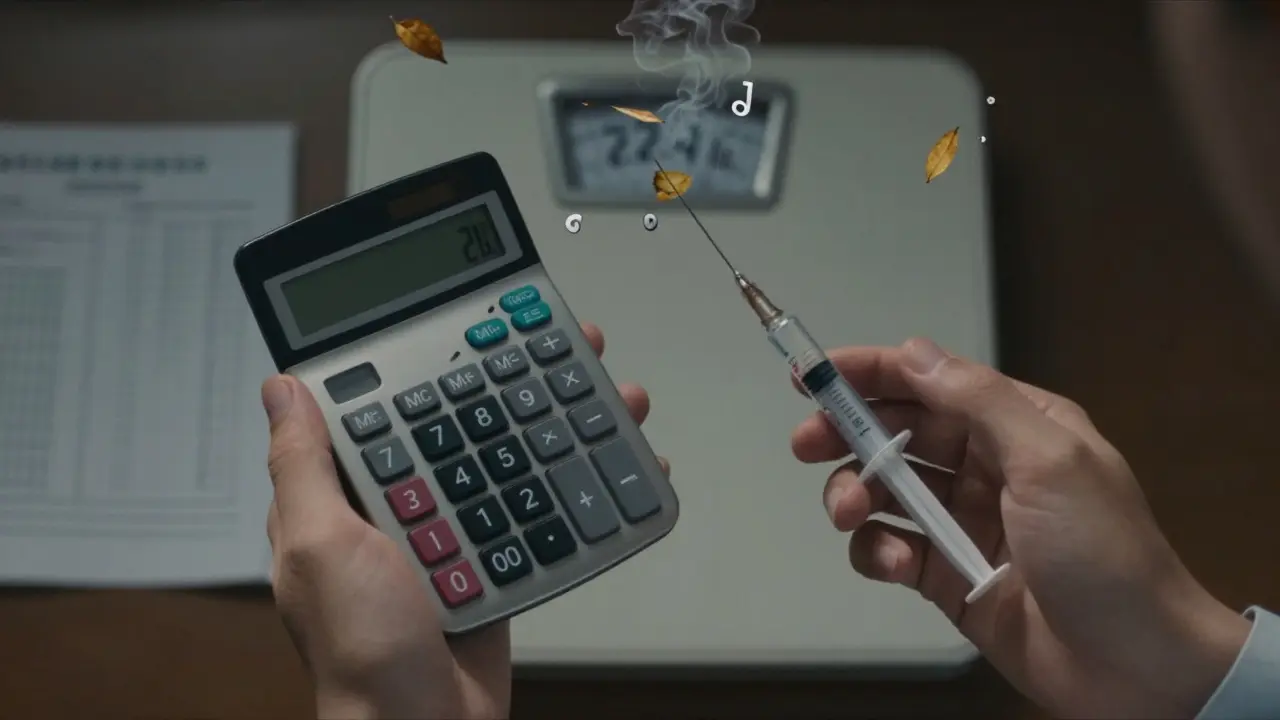
When a child gets sick, giving the right dose of medicine isn’t just about following a prescription-it’s a matter of life and death. Kids aren’t small adults. Their bodies process drugs differently, and a dose that’s safe for a 150-pound adult could be deadly for a 22-pound toddler. That’s why weight-based dosing is the gold standard in pediatric care today. It’s not a suggestion. It’s the rule. And it only works when paired with a strict double-check protocol.
Why Weight Matters More Than Age
For years, doctors guessed pediatric doses based on age. A child who was 2 years old got the same dose as another 2-year-old, even if one weighed 25 pounds and the other weighed 40. That approach led to dangerous mistakes. A 2022 study in Pediatrics found that age-based dosing had a 29% error rate in children at the extremes of growth. That means nearly 3 out of every 10 kids got the wrong dose just because someone assumed age = weight. Weight-based dosing fixes that. Instead of guessing, you calculate the dose using the child’s exact weight in kilograms. The formula is simple: weight (kg) × prescribed dose (mg/kg). For example, if a child weighs 10 kg and the order says 40 mg/kg/day of amoxicillin, the total daily dose is 400 mg. If it’s given twice a day, each dose is 200 mg. That’s precise. That’s safe. The American Academy of Pediatrics updated its guidelines in March 2022 to say that using weight instead of age cuts medication errors by 43%. That’s not a small improvement. It’s a lifesaver.The Three Steps to Get It Right
Getting the math right takes three steps-and skipping one can cause a serious error.- Convert pounds to kilograms correctly. Use the exact conversion: 1 kg = 2.2 lb. Never round until the very end. If a child weighs 22.4 pounds, divide by 2.2 to get 10.1818 kg. Keep all decimals until the final calculation. Rounding too early? That’s how 32% of dosing mistakes happen, according to the Institute for Safe Medication Practices (ISMP).
- Calculate the total daily dose. Multiply the child’s weight in kg by the prescribed dose per kg per day. For instance, 10.18 kg × 40 mg/kg/day = 407.2 mg/day.
- Divide by frequency. If the medication is given twice daily, divide the total daily dose by 2. So 407.2 mg ÷ 2 = 203.6 mg per dose. That’s the amount to give.
Why Double-Checks Save Lives
One nurse, Maria Chen, shared a story on AllNurses about a near-fatal error last year. A resident ordered 200 mg of a drug for a 10 kg child. The correct dose? 20 mg. That’s a 10-fold overdose. But the pharmacy double-checked the calculation and caught it. Why? Because the calculated dose exceeded the maximum safe limit of 40 mg/kg/day. That’s the power of a second set of eyes. The American College of Clinical Pharmacy found that independent double verification reduces serious pediatric medication errors by 68%. That’s not luck. That’s a system. Here’s how it works in practice:- One provider calculates the dose based on weight.
- A second provider recalculates it independently.
- They compare results. If they don’t match, they stop and figure out why.
When Weight Isn’t Enough
Weight-based dosing works for most kids. But not all. Some children need special adjustments. For example, obese children (BMI ≥95th percentile) have more body fat and less lean muscle. For water-soluble drugs like antibiotics, using actual weight can lead to overdose. The Pediatric Endocrine Society recommends using adjusted body weight:Adjusted Body Weight = Ideal Body Weight + 0.4 × (Actual Weight − Ideal Body Weight) A 2023 survey by the Children’s Hospital Association found that 78% of hospitals now use this method for certain drugs. It’s not common knowledge. But it’s becoming standard. Premature infants and babies under 6 months are another exception. Their livers and kidneys aren’t fully developed. A 5 kg baby might need 40-60% less of a drug like gentamicin than a 5 kg toddler-even though the math says the same dose. That’s not about weight. That’s about development. Ignoring this can cause hearing loss or kidney damage.
Common Mistakes and How to Avoid Them
Even experienced providers make mistakes. The ISMP’s 2023 report on pediatric errors shows the top three:- Unit confusion (38%): Mixing up pounds and kilograms. One nurse on Reddit said her hospital put bright red stickers on all scales that say: “WEIGH IN KG ONLY.” Now, errors dropped by 60%.
- Decimal point errors (27%): Writing 2.0 mg instead of 20 mg. Or worse, 200 mg instead of 20 mg. Always write doses with a leading zero (0.5 mg) and never a trailing one (5.0 mg).
- Ignoring organ function (19%): Giving the same dose to a child with kidney disease as one who’s healthy. Always check labs. Adjust for renal or liver impairment.

What’s Changing in 2026
The field is evolving fast. In 2023, Epic Systems rolled out pediatric-specific dosing modules in their EHR. These tools auto-calculate weight-based doses, check against institutional limits, and block unsafe orders. By 2026, 78% of children’s hospitals have them installed. The NIH’s Pediatric Trials Network has enrolled over 15,000 children to build better dosing guidelines for common drugs. And by 2025, the FDA will require all new drug applications to include pediatric dosing algorithms. But the foundation hasn’t changed. Weight-based dosing remains the backbone of pediatric medication safety. As Dr. Gregory Kearns of the Pediatric Pharmacology Research Unit Network said in 2023: “While precision dosing through therapeutic drug monitoring will increase, weight-based calculations will remain the essential foundation of pediatric pharmacotherapy for the foreseeable future.”What You Need to Remember
- Always use weight in kilograms-not pounds, not age.
- Convert pounds to kilograms without rounding until the final step.
- Always calculate the total daily dose, then divide by frequency.
- For high-alert drugs, require two independent calculations.
- Adjust for obesity, prematurity, or organ failure-weight alone isn’t always enough.
- Use technology, but never rely on it blindly. Know how to do the math by hand.

