Pediatric Medication Safety Calculator
Accurate weight conversion is critical for pediatric safety. A single pound-to-kilogram error can cause a 2.2x overdose before medicine even leaves the pharmacy.
Weight Conversion
Medication Safety Alert
Example: A 10 lb child (4.5 kg) receiving an adult dose could receive 2.2x the correct amount if weight is measured in pounds.
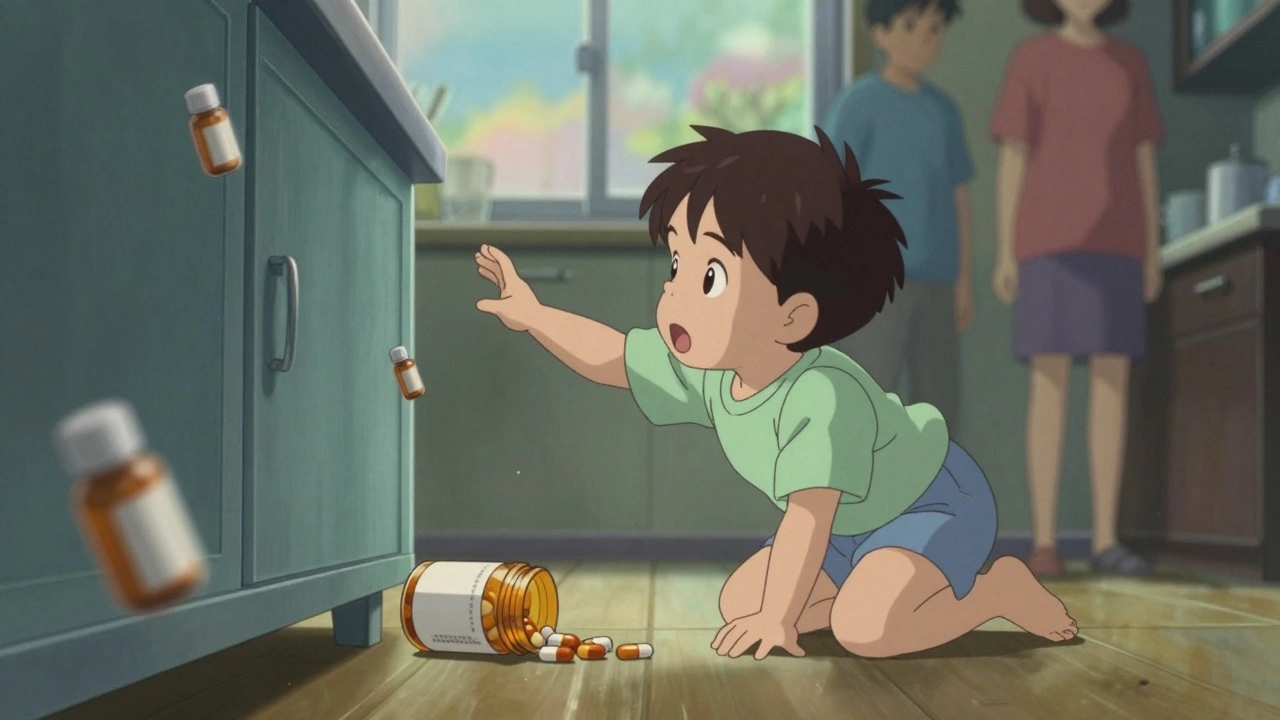
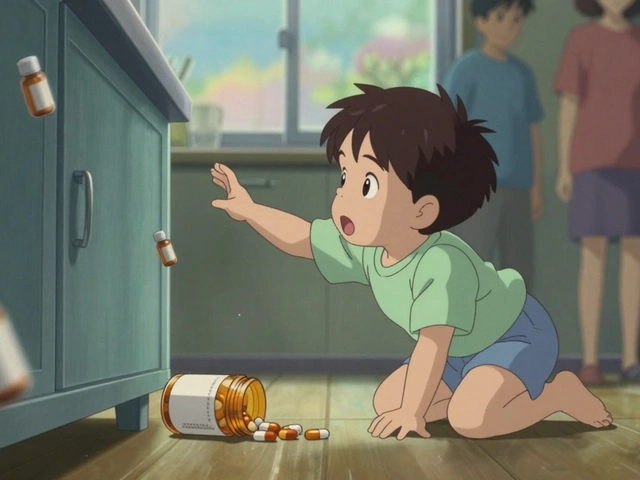
Every year, 50,000 children under age 5 end up in emergency rooms because they got into medicine they weren’t supposed to. Many of these cases aren’t accidents-they’re preventable mistakes. Parents think they’re being careful: the bottle is on the counter, the vitamins are in the drawer, the cough syrup is within reach for quick use at night. But children don’t need much time-or much strength-to get to medicine. In less than a minute, a curious toddler can open a bottle, swallow a pill, and be in serious danger.
Why Kids Are Different
Children aren’t small adults. Their bodies process medicine differently, and that’s not just a minor detail-it’s life-or-death. A dose that’s perfectly safe for a 150-pound teen could kill a 15-pound infant. This isn’t theoretical. Studies show pediatric medication errors happen about three times more often than in adults.Why? First, weight matters. Babies weigh 1-2 kilograms. Teens might weigh 60+ kilograms. That’s a 60-fold difference in body size. Dosing isn’t just “half the adult dose.” It’s calculated down to the milligram based on exact weight. Even a small mistake-like confusing pounds for kilograms-can lead to a 2.2x overdose before the medicine even leaves the pharmacy.
Second, their organs are still growing. A child’s liver and kidneys can’t clear medicine the way an adult’s can. That means drugs stay in their system longer, building up to toxic levels even at “correct” doses. A medicine that’s fine for an adult might cause liver damage or seizures in a 2-year-old.
Third, kids can’t tell you what’s wrong. If they feel dizzy, nauseous, or drowsy, they might just cry or curl up. They don’t say, “My head hurts,” or “I feel weird.” That delay means problems go unnoticed until it’s too late.
Common Mistakes That Put Kids at Risk
Some errors are simple, but deadly. Giving 1 teaspoon of medicine when the label says 1 milliliter? That’s a 5x overdose-because 1 teaspoon equals 5 milliliters. Give a tablespoon instead of a teaspoon? That’s a 3x overdose. These aren’t rare blunders. They happen every day because people still use kitchen spoons to measure medicine.
Another big problem: removing pills from child-resistant containers. Adults do it to make things easier-putting pills in a pill organizer, tossing them in a purse, or leaving them on the nightstand. But kids are smart. A 2020 study found that 45% of pediatric poisonings involved pills taken from containers that were once child-resistant-but now open because the cap wasn’t fully secured.
And don’t forget: it’s not just prescription drugs. Over-the-counter cough syrups, vitamins, diaper rash cream, eye drops, and even prenatal vitamins can be fatal to small children. A single pill of an adult heart medication can stop a baby’s heart. A few drops of liquid iron supplement can cause organ failure.
What Hospitals Do Right
Hospitals that treat kids regularly have learned the hard way. The American Academy of Pediatrics laid out 15 key safety steps in 2018, and the best children’s hospitals now follow most of them:
- Only use kilograms for weight-never pounds. Electronic systems block entry in pounds to prevent conversion errors.
- Standardize concentrations of high-risk drugs like insulin or morphine. No more “10 mg/mL” vs. “100 mg/mL” confusion.
- Require two independent checks for high-alert medications before giving them to a child.
- Create “distraction-free zones” where nurses prepare meds-no phones, no chatter, no interruptions.
- Use milliliter-only dosing devices for home use. No teaspoons. No tablespoons. Only syringes or cups marked in mL.
These aren’t suggestions. They’re proven. Facilities that follow these rules cut pediatric medication errors by 85%.

What You Need to Do at Home
Hospital protocols won’t help if the medicine is sitting on the kitchen counter at home. Here’s what you need to do:
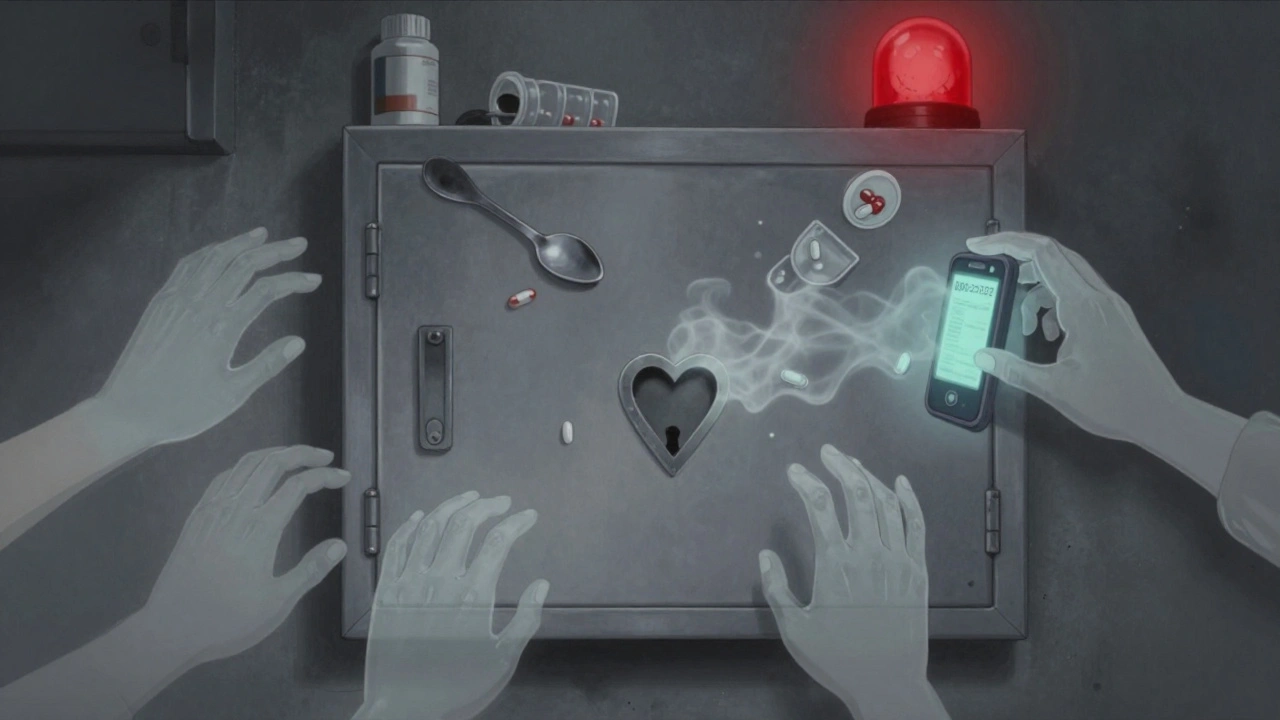
- Store all medicine up and away-not on the counter, not in a drawer your child can open, not in your purse. Use a locked cabinet or high shelf. The CDC says 75% of poisonings happen because parents thought the storage spot was “safe.”
- Never tell a child medicine is candy. Even if you say it “tastes like candy,” it plants the idea that medicine is a treat. That’s linked to 15% of accidental ingestions.
- Always close child-resistant caps properly. If the cap isn’t clicked or locked, it’s open. Kids can open half-closed caps in under 30 seconds.
- Use only the dosing tool that comes with the medicine. If it’s a syringe, use the syringe. If it’s a cup, use the cup. Never guess with a kitchen spoon.
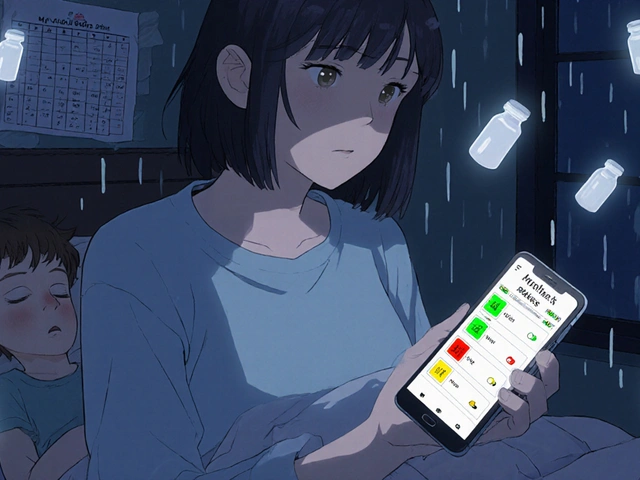
- Administer liquid medicine against the cheek, not the tongue. This helps avoid choking and ensures the full dose is swallowed.
- Treat all products like medicine. That includes vitamins, eye drops, topical creams, and even alcohol-based hand sanitizers. All of them have caused poisonings.
What to Do If Your Child Gets Into Medicine
Don’t wait. Don’t call your pediatrician first. Don’t try to make them throw up. Call Poison Help immediately: 800-222-1222. Program that number into your phone, your home phone, and your kids’ tablets if they have one. Save it as “Poison Help” so anyone can find it.
Have the medicine container ready when you call. Tell them what was taken, how much, and when. Don’t guess. Even if you’re not sure, call anyway. Poison control centers handle over 1 million pediatric cases a year. They know what to do.
Why This Matters Now More Than Ever
Medicine is more accessible than ever. Online pharmacies deliver pills to your door. Pain patches, opioid tablets, and liquid sedatives are common in homes. The FDA now requires new pediatric drugs to come in standardized concentrations to reduce errors-but that doesn’t help with older medicines already in your cabinet.
And while hospitals are getting better, most pediatric poisonings happen at home. The CDC’s PROTECT Initiative, launched in 2010, continues to update guidelines every year. Their latest advice? Use pictogram-based dosing sheets. Studies show they improve accuracy by 47% for parents with low health literacy.
Teach-back is another powerful tool. After your doctor or pharmacist explains how to give the medicine, ask them to watch you do it. Say, “Can I show you how I’ll give this to my child?” If you can do it right, you’ve understood. If you hesitate, ask again.
Final Thoughts
Pediatric medication safety isn’t about being perfect. It’s about building habits that reduce risk. One wrong teaspoon. One open bottle. One moment of distraction. That’s all it takes.
Check your home right now. Where is the medicine? Is it locked? Is the cap on tight? Are you using the right tool to measure? Are you telling your child it’s candy? If you’re not sure, fix it today. You won’t regret it.
Medicine saves lives. But only when it’s used correctly. For children, that means being more careful than you’ve ever been before.