Getting the right dose of medicine for a child isn’t just tricky-it’s life-or-death. A wrong number, a misread label, or a confused schedule can turn a routine treatment into a medical emergency. Unlike adults, kids don’t get standard doses. Their weight, age, and even developmental stage change how much medicine they need. One pill too much, and you risk toxicity. One pill too little, and the infection won’t clear. That’s why tracking pediatric doses with apps and dosing charts isn’t a convenience-it’s a necessity.
Why Pediatric Dosing Is So Dangerous
Pediatric medication errors happen up to three times more often than in adults, according to the Institute for Safe Medication Practices. Why? Because calculations are complex. A typical dose might be 10 mg per kilogram of body weight. If you don’t know how to convert pounds to kilograms, or if you misread the scale, you’re already off track. Manual calculations take time. In a busy ER or at 2 a.m. with a feverish toddler, that delay can cost you clarity. And when parents are juggling multiple medications, missed doses, or overlapping schedules, the risk multiplies.One parent in a 2023 survey told researchers they accidentally gave their 22-month-old three times the recommended dose of ibuprofen because they entered the child’s weight in pounds instead of kilograms in a free app. The child ended up in the hospital. That’s not a rare mistake. It’s a predictable one.
Apps for Clinicians: Speed, Accuracy, and Safety
In hospitals and clinics, professionals rely on tools built for high-stakes environments. Pedi STAT, developed by emergency medicine doctors at Connecticut Children’s Medical Center, was one of the first apps made just for pediatric emergencies. It’s designed for speed: enter a child’s weight in kilograms, tap once, and it calculates doses for 15+ emergency drugs-epinephrine, albuterol, acetaminophen-in under three seconds. That’s 15 seconds faster than doing it by hand, and with error rates down from 12% to under 3%.Another staple is Epocrates. It’s not just for kids-it covers 4,500+ medications across all ages. What makes it powerful is its drug interaction checker. If a child is on two meds that shouldn’t mix, it flags it before the nurse even opens the bottle. It’s used in 89% of U.S. children’s hospitals. But it’s not free. The full version costs $175 a year. Many clinics pay for it. Parents don’t.
Then there’s PedsGuide from Children’s Mercy Kansas City. It’s used by clinicians for complex cases, like neonatal ICU patients or kids on IV drips. It includes equipment sizing (like endotracheal tubes) based on height, and it’s FDA-cleared as a medical device. But here’s the catch: it’s locked behind hospital licenses. Parents can’t download it. It’s meant for staff only.
Apps for Parents: Simplicity and Peace of Mind
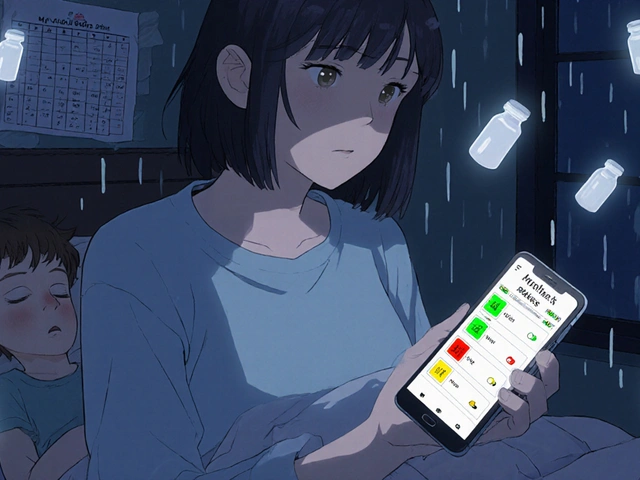
At home, parents need something different. They don’t need drug interaction tables or IV infusion rates. They need reminders, visual cues, and a way to avoid giving the same medicine twice.My Child’s Meds is the most trusted app for families. Developed with input from the Royal College of Paediatrics and Child Health and WellChild, it lets you add each child’s medications with exact dosages, times, and instructions. It sends alerts when it’s time to give a pill, and it blocks you from entering a second dose within the safe window. One parent shared that it prevented a potential overdose during night feedings when her toddler’s schedule got mixed up. The app uses color-coded icons-green for on time, red for missed, yellow for late-so even a tired parent can glance at the screen and know what’s happening.
Another favorite is NP Peds MD. It doesn’t calculate doses. Instead, it shows clear, pediatrician-approved charts for common OTC meds like acetaminophen and ibuprofen. You find your child’s weight, and it tells you the exact amount to give. No math. No guesswork. Just a table you can print or screenshot. In a Consumer Reports test, 78% of parents using this app gave the right dose-compared to just 52% using printed paper charts.
These apps are free or one-time purchases. My Child’s Meds is $0. NP Peds MD is free. No subscriptions. No hidden fees. That’s critical-parents shouldn’t have to pay to keep their kids safe.

The Big Problem: Apps Don’t Talk to Each Other
Here’s where things fall apart. When a child leaves the hospital, the doctor hands over a paper sheet with dosing instructions. The parent opens My Child’s Meds and types it all in by hand. But the hospital’s system used Pedi STAT. The pharmacy used a different app. None of these tools share data. That’s why 87% of medication errors in kids happen during care transitions-from hospital to home, or from ER to pediatrician.Parents report spending hours trying to match what the nurse said with what the pharmacist wrote and what the app suggests. One mom told a researcher she had three different charts for her son’s asthma meds-each with slightly different times. She ended up giving the wrong dose three days in a row.
Even worse, some apps on the Google Play Store claim to be dose calculators but are just glorified note-takers. They don’t check for safety limits. They don’t warn about double dosing. One app called Child Medical History costs $3.99 and only lets you log meds-it can’t calculate anything. Parents think they’re getting a safety tool. They’re not.
What Works Best: Best Practices for Safe Dosing
No app is perfect. Even the best ones can fail if you don’t use them right. Here’s what actually keeps kids safe:- Always check the unit. Kilograms or pounds? If the app asks for weight, make sure you’re entering the right one. Most errors come from mixing them up.
- Double-check the math. Even if the app says 15 mL, look at the dosing chart on the bottle. Does it match? If not, call your pharmacist.
- Use paper backups. When the phone dies, the app crashes, or the Wi-Fi goes out, you need a printed copy. Keep one taped to the fridge.
- Reconcile weekly. Every Sunday, compare your app’s log with your pharmacy’s record. Did they refill the same amount? Is the dose still right as your child grows?
- Teach everyone who gives meds. Grandparents, babysitters, nannies-they all need to know how the app works. Don’t assume they’ll figure it out.
Children’s Hospital of Philadelphia recommends parents do a “medication reconciliation” with their pharmacy every week. It takes five minutes. It can prevent a trip to the ER.
The Future: Where This Is Headed
The next big step? Apps that talk to each other. The Healthcare Information and Management Systems Society (HIMSS) is working on a standard that will let hospital apps send dosing info directly to parent apps-securely, automatically. Trials are already running in Boston and Chicago. By 2027, this could be the norm.Some apps are testing AI that predicts when a parent is likely to make a mistake-like if they’re entering a dose at 3 a.m. or if they’ve missed two doses in a row. Smart pill dispensers that sync with apps are being tested too. Imagine a device that only opens when it’s time for the right dose-and sends a text to your phone if you try to open it early.
But technology alone won’t fix this. Training matters. Clinicians need to teach parents how to use the tools. Parents need to understand why the numbers matter. The NIH study on Peda Karmania found that apps with simple, intuitive design cut errors by 43%. But only if users actually understood how they worked.
What to Do Today
If you’re a parent:- Download My Child’s Meds (iOS) or NP Peds MD (iOS and Android).
- Enter every medication, including vitamins and supplements.
- Set reminders for every dose.
- Print a backup chart and keep it with the meds.
- Don’t use free apps that don’t come from trusted health organizations.
If you’re a provider:
- Recommend My Child’s Meds or NP Peds MD to families.
- Don’t assume parents know how to use the apps-show them.
- Use Pedi STAT or Epocrates in your practice. Train new staff.
- Advocate for interoperability with your IT team.
Medication safety for kids isn’t about having the fanciest app. It’s about using the right tool, the right way, every single time.
Can I use any medication app for my child?
No. Not all apps are safe. Avoid apps that don’t come from hospitals, pharmacies, or major health organizations. Free apps from unknown developers often lack safety checks and can give dangerously wrong doses. Stick to apps like My Child’s Meds, NP Peds MD, or those recommended by your pediatrician. Look for endorsements from groups like the Royal College of Paediatrics and Child Health or the American Academy of Pediatrics.
Do I still need to check the bottle if the app says the dose is right?
Yes, always. Apps can have bugs, outdated databases, or input errors. The bottle or prescription is your final safety check. Compare the app’s suggestion with the label on the medicine. If they don’t match, call your pharmacist before giving the dose. Never rely on one source alone.
What if my child’s weight changes?
Update the weight in your app every time your child has a checkup. Doses are based on weight, not age. Even a 2-pound gain can change the right amount for some medications. If you’re unsure, ask your doctor or pharmacist to recalculate the dose. Don’t guess.
Are these apps HIPAA-compliant?
Professional apps like Pedi STAT and Epocrates are HIPAA-compliant because they’re used in clinical settings. Most parent apps like My Child’s Meds are not required to be HIPAA-compliant because they’re classified as general wellness tools. That means your child’s data isn’t protected under federal privacy law. Don’t store sensitive medical records in them unless you’re sure they encrypt data. Always check the app’s privacy policy.
Can I use a dosing chart instead of an app?
Yes, and many parents do. Printed dosing charts from trusted sources like the American Academy of Pediatrics or your child’s hospital are reliable. But apps add reminders, error-blocking features, and history logs that paper can’t. If you use paper, make sure it’s clear, up-to-date, and kept where everyone can see it. Consider using both: the chart as backup, the app as your daily guide.