Every year, over 350,000 older adults end up in the hospital because of medication mistakes-most of them preventable. Seniors take more drugs than any other group. About 90% of people over 65 use at least one prescription, and 40% take five or more daily. Add in vitamins, supplements, and over-the-counter pain relievers, and it’s easy to lose track. For caregivers, it’s even harder. One missed dose, one wrong combination, one pill stored in the wrong place-and a small error can lead to a fall, a trip to the ER, or worse. But it doesn’t have to be this way. With a few clear, practical steps, you can cut the risk dramatically.
Keep a Complete, Updated Medication List
Don’t rely on memory. Not even close. Write down every single thing the senior takes-prescription, over-the-counter, herbal, vitamin, or supplement. Include the exact name, dosage, how often it’s taken, why it was prescribed, the doctor’s name, and the pharmacy’s phone number. Also note when it was started and any known side effects. The Health in Aging Foundation says this list needs all 10 details to be truly useful.Update this list within 24 hours of any change. If the doctor adds a new pill or stops one, change the list right away. Bring this list to every appointment-even a routine check-up. Pharmacists say 92% of dangerous drug interactions are caught just by seeing this updated list. Many seniors keep their list in a wallet, taped inside a medicine cabinet, or saved on their phone. But if the phone dies or the wallet gets lost, you’re back to guessing. Print two copies. One stays with the senior. One stays with the caregiver.
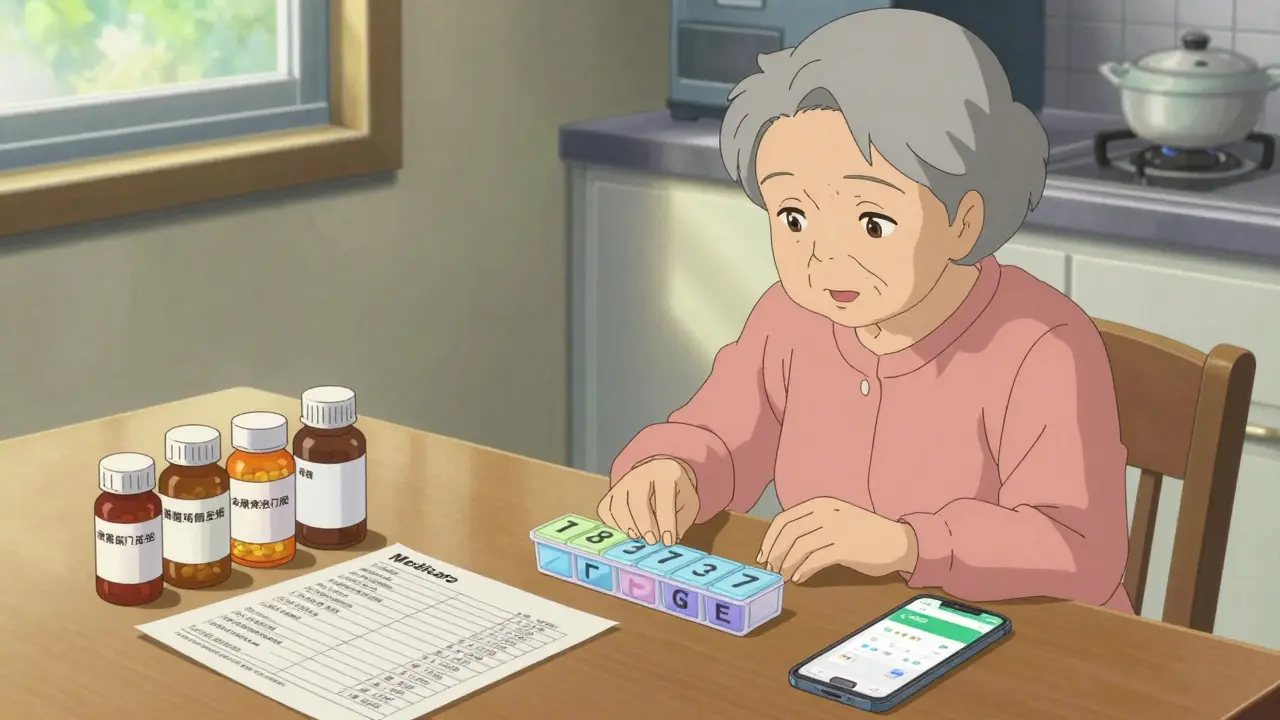
Use a Pill Organizer-But Choose the Right One
Pill organizers aren’t just helpful; they’re lifesavers. A color-coded, 7-day AM/PM organizer can improve adherence by nearly 50% in seniors with mild memory issues, according to the National Institute on Aging. But not all organizers work the same. A simple one-compartment box won’t cut it if someone takes meds at breakfast, lunch, dinner, and bedtime.Start simple. If the senior takes meds only once or twice a day, a single-compartment weekly organizer is fine. If they take multiple doses daily, go for a 7-day, 4-compartment (morning, noon, evening, night) box. Look for ones with large print labels and easy-to-open lids. Some have alarms built in. Others are locked-great if the person tends to take extra doses by accident.
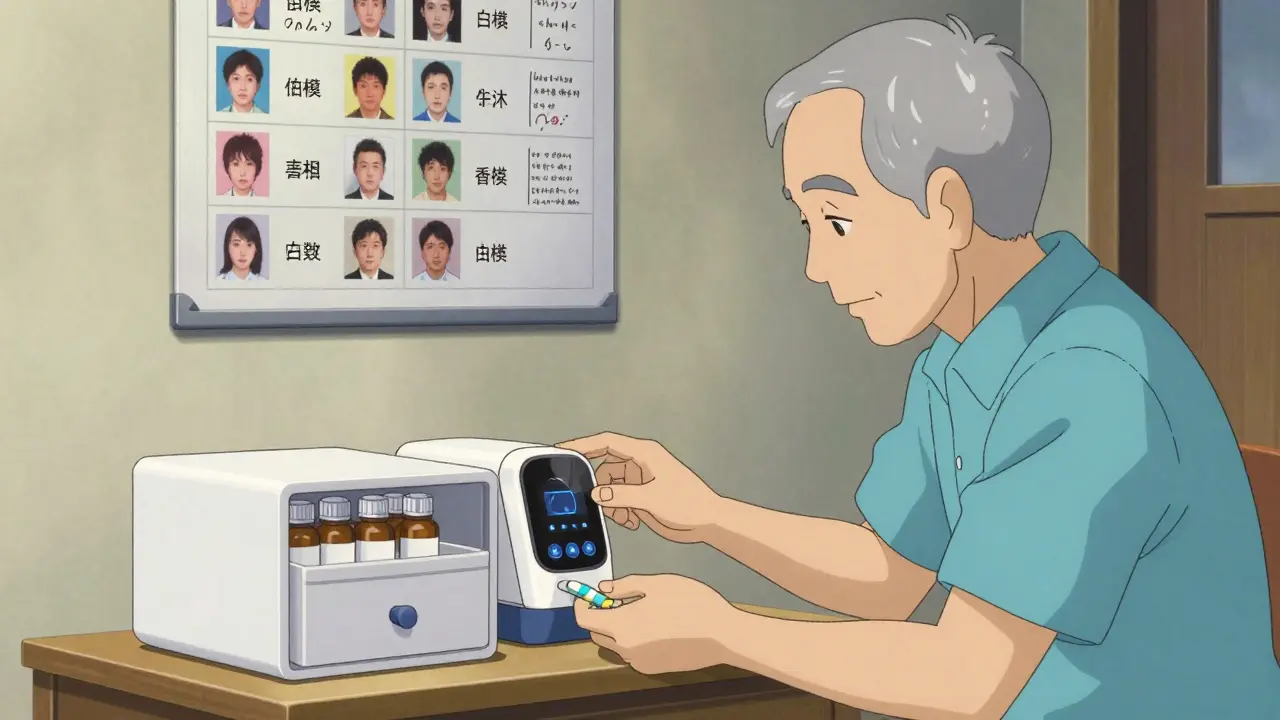
One caregiver in Dunedin told me her mother kept doubling up on her blood pressure pill because she couldn’t remember if she’d already taken it. After switching to a locked organizer, missed doses dropped from 40% to 5% a month. But if the senior has advanced dementia, even a locked organizer might not be enough. That’s when digital tools like Medisafe or Hero come in. Medisafe sends phone alerts and tracks whether pills were taken. Hero is a smart dispenser that releases pills only at the right time and texts caregivers if a dose is skipped. Studies show these tools boost adherence from 55% to 89%. But they’re not foolproof. Some seniors ignore alerts or override safety features. The key? Test it. Watch how they use it for a week before committing.
Check for Dangerous Interactions
It’s not just about what’s in the pill-it’s what’s in the glass. Grapefruit juice interacts with 85 common medications, including statins and blood pressure drugs. Alcohol mixes dangerously with 150+ medications, especially sedatives, diabetes pills, and painkillers. Even something as simple as St. John’s Wort can cancel out antidepressants or birth control.The American Geriatrics Society updates the Beers Criteria® every two years. It’s a list of 138 medications that are risky for seniors because they cause confusion, falls, or kidney damage. Common offenders include certain sleep aids, antihistamines, and NSAIDs like ibuprofen. If your loved one is taking any of these, ask the doctor: “Is this still necessary?”
Deprescribing-cutting back on unneeded meds-is one of the most powerful safety moves. A 2022 study showed that when doctors systematically reduced medications in seniors taking 10 or more, falls dropped by 22% and hospital visits fell by 18%. Don’t stop meds on your own. But do ask: “Can we reduce this?” “Is there a safer alternative?” “What happens if we stop it?”
Store Medications Properly
The bathroom medicine cabinet is the worst place to store pills. Steam, heat, and moisture destroy medication. A 2022 University of Florida study found that 37% of common drugs lose potency when stored in a humid bathroom. Heat above 86°F (30°C) can break down insulin, thyroid meds, and nitroglycerin. Cold can ruin some liquid antibiotics.Keep all medications in their original bottles, with labels intact. Store them in a cool, dry place-like a bedroom drawer or kitchen cabinet away from the stove. Temperature should stay between 68-77°F (20-25°C). Humidity under 60% is ideal.
And lock them up. Nearly 60,000 children are treated each year for accidental poisoning from meds left within reach. If grandchildren visit, even occasionally, a locked box is non-negotiable. Many pharmacies offer free childproof locks for pill bottles. Ask for them.
Talk to the Doctor-The Right Way
Doctors are busy. Caregivers are overwhelmed. But if you don’t ask the right questions, mistakes happen. Prepare three questions for every appointment:- “Is this medication still needed?”
- “What interactions should I watch for?”
- “Are there cheaper or safer alternatives?”
Also ask: “What are the signs of a dangerous side effect?” For example, if someone takes a blood thinner, they should know that unusual bruising, dark stools, or headaches could mean internal bleeding. If they’re on diabetes meds, confusion or shaking could signal low blood sugar.
The Alzheimer’s Association found that using this structured approach cuts medication errors by 63% in dementia patients. Don’t wait for the appointment. Call the pharmacist. They’re trained to catch interactions and can review all meds at once. Medicare Part D offers free Medication Therapy Management (MTM) for people taking 8+ chronic meds. Ask if you qualify.
And if you’re overwhelmed? Use the NIA’s free ‘Medication Check-Up’ program. It’s available through 11,000 Area Agencies on Aging across the U.S. A trained pharmacist comes to the home, reviews every pill, and gives you a clear plan. No cost. No pressure. Just help.

Common Mistakes to Avoid
Many caregivers make the same errors-over and over. Here’s what to skip:- Crushing pills. Time-release or enteric-coated pills can become dangerous if crushed. Always ask before breaking a tablet.
- Keeping expired meds. The average senior home has $317 worth of old, unused, or expired drugs. They take up space, create confusion, and can be toxic if taken accidentally. Dispose of them safely at a pharmacy take-back program.
- Skipping refills. Running out of a blood pressure or heart med for even a day can cause a spike in risk. Set phone reminders or sign up for automatic refills.
- Using multiple pharmacies. Each pharmacy has its own system. If you use two, they can’t see what the other is dispensing. Stick to one pharmacy so they can flag interactions.
One caregiver in New Zealand told me she made a laminated chart with photos of each pill next to its name and purpose. Her dad, who struggled with unfamiliar pills, stopped refusing meds after seeing the pictures. He said it made him feel more in control. Simple. Cheap. Effective.
What Works Best? Real Stories
There’s no one-size-fits-all. Some seniors thrive with apps. Others need paper. A 2023 AARP survey found 55% of seniors over 75 prefer written schedules. But 73% said large-print pill organizers gave them confidence. The key is matching the tool to the person.One man in his 80s with early dementia used a simple weekly pill box with a sticky note on top: “Take before breakfast.” He didn’t need an app. He just needed clarity. Another woman used Hero’s smart dispenser. Her daughter got alerts if the dose wasn’t taken-and could call the pharmacy to refill automatically. Both worked. Both saved lives.
The goal isn’t perfection. It’s progress. Even reducing missed doses from 40% to 10% is a win. If you’re feeling stuck, reach out. Talk to a pharmacist. Call your local Area Agency on Aging. Ask for help. You’re not alone.
What should I do if my loved one forgets to take their medication?
First, don’t panic. Never double the dose unless the doctor says so. Use a pill organizer with alarms or a smart dispenser like Hero or Medisafe that alerts caregivers. If missed doses happen often, talk to the doctor about simplifying the regimen-maybe switching from four times a day to once daily. Many seniors do better with fewer pills, taken at the same time each day.
Can I mix over-the-counter meds with prescriptions?
Not without checking. Many OTC drugs like ibuprofen, antihistamines, and cold medicines interact with prescriptions. For example, ibuprofen can raise blood pressure and harm kidneys in seniors on heart or kidney meds. Antihistamines can cause dizziness and confusion. Always tell your pharmacist or doctor every OTC product you’re using-even if you think it’s harmless.
How do I know if a medication is expired?
Check the expiration date on the bottle or box. If it’s past that date, don’t use it. Some meds, like insulin or liquid antibiotics, lose effectiveness quickly after expiration. Others, like tablets, may still be safe for a short time-but potency drops. The FDA says it’s not worth the risk. Dispose of expired meds at a pharmacy take-back program. Never flush them unless the label says to.
Is it safe to store medications in the fridge?
Only if the label says so. Most pills are fine at room temperature. But some, like insulin, certain eye drops, or liquid antibiotics, need refrigeration. Keep them in the main compartment, not the door, where temperature changes. Always check the instructions. If in doubt, call the pharmacy. Storing meds in the fridge unnecessarily can damage them.
What if my loved one refuses to take their meds?
Don’t force it. Try to understand why. Is it because of side effects? Confusion? Fear? Taste? Sometimes, changing the form helps-like switching from a pill to a liquid. Or ask the doctor if a different brand or generic version is available. Use visual cues: show them the pill, say its name, and explain why it’s important. A laminated photo chart can help. If resistance continues, talk to the doctor. There may be a safer alternative or a way to simplify the regimen.
If you’re managing medications for a senior, you’re doing something vital. It’s not glamorous. But it’s one of the most powerful ways to protect their health, independence, and peace of mind. Start with one tip. Get the list updated. Then add the organizer. Then ask one question at the next doctor’s visit. Small steps. Big results.