Glaucoma doesn’t hurt. It doesn’t blur your vision suddenly. It doesn’t make your eyes red or watery. That’s why it sneaks up on you. By the time you notice something’s wrong, the damage is often permanent. It’s called the silent thief of sight for a reason.
What Exactly Is Glaucoma?
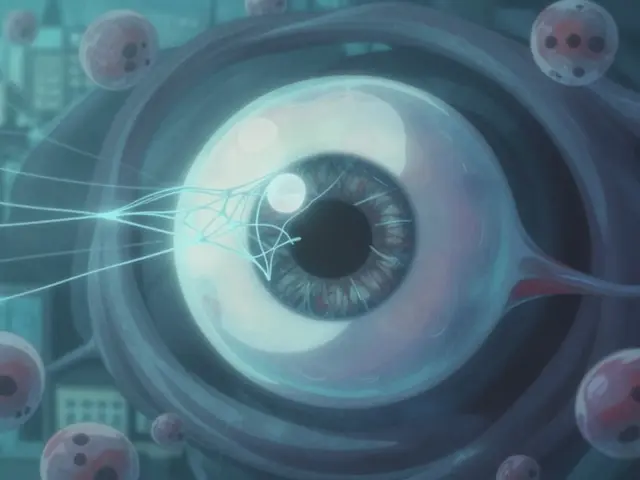
Glaucoma isn’t just high eye pressure. That’s the old belief - the one doctors held for over a hundred years. Today, we know it’s more complex. Glaucoma is a group of diseases that damage the optic nerve, the cable that sends visual information from your eye to your brain. The damage usually starts at the back of the eye, where the optic nerve exits the eyeball. That spot is called the optic nerve head. When it gets injured, you lose peripheral vision first - the edges of what you see. You might bump into doorframes, miss steps, or not notice someone standing to your side. But your central vision? That stays sharp until late stages. By then, it’s too late to reverse what’s lost.High Eye Pressure Isn’t Always the Culprit
Most people think if your eye pressure is normal, you’re safe. That’s not true. Normal eye pressure ranges from 10 to 21 mmHg. But about 30% of glaucoma patients have pressures right in that normal range. That’s called normal-tension glaucoma. It’s more common in Asian populations and can be just as damaging as high-pressure glaucoma. So why does damage happen even when pressure is normal? It’s not just about the number on the tonometer. It’s about the pressure difference between your eye and your brain. Your eye has pressure (intraocular pressure, or IOP). Your brain has pressure too (intracranial pressure, or ICP). The gap between them - the translaminar pressure difference - matters more than either number alone. In glaucoma patients, ICP is often lower than normal. That means even a normal IOP can push harder on the optic nerve than it should. Think of it like a balloon inside a jar. If the air pressure outside the jar drops, the balloon expands even if you don’t add more air inside.How the Damage Actually Happens
Inside the optic nerve head is a sponge-like structure called the lamina cribrosa. It’s made of collagen fibers that let nerve fibers pass through. When pressure builds up - whether from high IOP, low ICP, or both - this mesh gets stretched. Studies show it can stretch up to 3% more in glaucoma eyes than in healthy ones. That strain crushes the tiny nerve fibers that carry vision signals. Over time, those fibers die. The cells that support them - astrocytes, microglia, fibroblasts - also get damaged. This isn’t just mechanical. Blood flow to the optic nerve can drop too. That means less oxygen and nutrients. The result? Retinal ganglion cells, the neurons that make up the optic nerve, slowly start to disappear. Once they’re gone, they don’t come back.Two Main Types of Glaucoma - And Why It Matters
There are two main types you need to know: open-angle and angle-closure. Open-angle glaucoma is the most common. About 90% of cases in the U.S. are this type. The drainage system in your eye - the trabecular meshwork - gets clogged over time. Fluid builds up. Pressure rises. It happens slowly. You won’t feel it. That’s why regular eye exams are critical. Angle-closure glaucoma is less common globally but more dangerous. It’s responsible for half of all glaucoma blindness in Asia. Here, the iris blocks the drainage angle suddenly. Pressure spikes fast - sometimes to 40 or 50 mmHg. This is an emergency. Symptoms include severe eye pain, nausea, blurred vision, halos around lights. If you feel this, get help immediately. Permanent vision loss can happen in hours.
How Doctors Diagnose It
No single test catches glaucoma. It takes three things:- Eye pressure measurement - using Goldmann applanation tonometry, the gold standard. It’s not just one reading. Pressure changes throughout the day. Peak pressure often hits between 6 and 8 a.m.
- Optic nerve imaging - optical coherence tomography (OCT) scans the nerve layer down to 5-10 microns. That’s thinner than a human hair. Thinning here means damage.
- Visual field testing - Humphrey perimetry checks your side vision. It finds tiny blind spots as small as 1 dB loss. That’s barely noticeable to you, but it’s the first sign of nerve loss.
Doctors also take photos of your optic disc. If the cup (the center of the disc) is growing larger over time, that’s a red flag. A cup-to-disc ratio over 0.6 in one eye - or asymmetry between eyes - raises concern.
Treatment Isn’t One-Size-Fits-All
The goal isn’t to get pressure to normal. It’s to get it low enough to stop further damage. That’s called your target IOP. It’s different for everyone.- For mild glaucoma: reduce pressure by 20-25% from baseline - often to 18-21 mmHg
- For moderate: 25-35% reduction - usually 15-18 mmHg
- For severe: 30-50% reduction - often down to 12-15 mmHg
First-line treatment? Prostaglandin eye drops like latanoprost. They lower pressure by 25-33% with just one drop a night. But they come with side effects: eyelashes get longer, darker, thicker. The skin around the eye can sink in. Some people hate the look.
If drops don’t work, laser treatment - selective laser trabeculoplasty - opens the drainage system. It works in 75% of people. But its effect fades. Each year, about 10% lose the benefit.
Surgery is next. Trabeculectomy creates a new drainage channel. It works well - 85% success at one year - but carries risks like infection and cataracts. Newer options, called MIGS (minimally invasive glaucoma surgery), like the iStent, are safer. They lower pressure by 20-25% and are often done at the same time as cataract surgery.
Why People Stop Taking Their Drops
Here’s the ugly truth: half of glaucoma patients stop taking their eye drops within a year. Why? Side effects. Burning, redness, blurry vision. Cost. Forgetting. And the biggest reason? They feel fine. No pain. No symptoms. So they think, “It’s working.” But glaucoma doesn’t care how you feel. It’s still eating away at your nerves.One patient on Reddit wrote: “My IOP is 12-13 mmHg. I’ve had it for five years. My vision is still getting worse.” That’s normal-tension glaucoma in action. Pressure isn’t the whole story. That’s why neuroprotective treatments are being tested. Drugs like brimonidine may protect nerve cells directly, even if pressure doesn’t drop much. Early studies show 30% slower progression in NTG patients.

The Future: Beyond Pressure Control
Scientists are no longer just lowering pressure. They’re trying to save the nerve itself.- Oncomodulin - a natural protein that helps nerve fibers regrow. In lab animals, it restored 40% of damaged axons.
- CNTF implants - tiny devices that slowly release a growth factor. In trials, they preserved 2.5 dB more vision over two years.
- Gene therapy - targeting the trabecular meshwork to improve drainage. Phase 1 trials show 25% IOP drop after six months.
- AI-powered OCT - machines now spot early glaucoma with 94% accuracy, even before doctors see changes.
Home monitoring is coming too. Contact lenses like Triggerfish can track pressure 24/7. They’re not perfect - ±1.5 mmHg accuracy - but they show when pressure spikes at night, when most damage happens.
Who’s at Risk?
You’re at higher risk if you:- Are over 60
- Have a family history of glaucoma
- Are African, Asian, or Hispanic
- Have diabetes, high blood pressure, or migraines
- Have had a serious eye injury
- Use steroid medications long-term
And here’s something few know: people with low intracranial pressure - like those with sleep apnea or chronic low blood pressure - are more vulnerable. It’s not just about your eyes. It’s about your whole body’s pressure balance.
What You Can Do
There’s no cure. But there is control.- Get a comprehensive eye exam every 1-2 years after 40. If you’re high-risk, start at 35.
- Don’t skip your eye drops. Set phone alarms. Use pill organizers.
- Exercise. Walking 20 minutes a day lowers IOP by 5-10 mmHg.
- Avoid inverted positions (like yoga headstands) - they spike eye pressure.
- Don’t smoke. It reduces blood flow to the optic nerve.
Glaucoma isn’t a death sentence. It’s a chronic condition - like high blood pressure. With early detection and consistent treatment, most people keep their vision for life. But if you wait until you can’t see the edge of your phone screen? It’s too late.
Can glaucoma be cured?
No, glaucoma cannot be cured. Once retinal ganglion cells die, they don’t regenerate. But with early detection and consistent treatment, progression can be slowed or stopped in most cases. The goal is to preserve remaining vision, not restore what’s lost.
If my eye pressure is normal, can I still have glaucoma?
Yes. About 30% of glaucoma cases occur with normal eye pressure (10-21 mmHg). This is called normal-tension glaucoma. Damage happens due to factors like low intracranial pressure, poor blood flow to the optic nerve, or genetic susceptibility. Normal pressure doesn’t mean safe pressure.
How often should I get tested for glaucoma?
If you’re over 40 with no risk factors, get a full eye exam every 2 years. If you’re over 60, or have family history, diabetes, or are African or Asian descent, get tested every year. If you’ve been diagnosed with glaucoma or ocular hypertension, your doctor will recommend testing every 3-6 months for pressure, annually for visual fields, and every 6-12 months for OCT scans.
Do glaucoma eye drops have serious side effects?
Yes, but they’re usually manageable. Prostaglandin analogs like latanoprost can darken eyelashes, cause eyelid skin to sink in, or change iris color. Beta-blockers like timolol can cause low heart rate or breathing issues in people with asthma. Most side effects are cosmetic or mild. The bigger risk is not using them - vision loss is permanent.
Can lifestyle changes help with glaucoma?
Yes. Regular aerobic exercise like walking or cycling lowers eye pressure. Avoid holding your breath or doing inverted poses (like headstands). Don’t smoke - it reduces blood flow to the optic nerve. Eat leafy greens - they’re rich in nitrates linked to better blood flow. Manage blood pressure and sleep apnea - both affect pressure balance in the eye and brain.
Is glaucoma hereditary?
Yes. Having a first-degree relative with glaucoma increases your risk by up to 10 times. If your parent or sibling has it, you should start annual eye exams by age 35, even if you feel fine. Genetic factors influence drainage system structure, optic nerve resilience, and how your body responds to pressure.