Every year, millions of people are harmed by the very medicines meant to help them. It’s not a rare accident-it’s a pattern. One in every 20 patients worldwide experiences avoidable harm from medication. That’s not a small number. That’s someone you know. Maybe it’s your parent, your neighbor, or even you. The truth is, medication safety isn’t just a hospital policy-it’s something every patient needs to understand and act on.
How Common Are Medication Errors?
Medication errors happen more often than most people realize. Globally, about 5% of patients are harmed by drugs each year. In the United States alone, over 1.3 million people suffer medication-related injuries annually. That’s more than the population of Dunedin, New Zealand-multiplied by 10. And it’s not just about side effects. Many of these are preventable mistakes: the wrong dose, the wrong drug, or a drug that shouldn’t have been prescribed at all.
These errors lead to at least 7,000 deaths in U.S. hospitals each year. One death per day. That’s not a statistic-it’s a family losing someone they love because a pill was mislabeled, a nurse misread a chart, or a patient didn’t understand the instructions. And it’s not just hospitals. Over 1.5 million emergency room visits in the U.S. each year are due to adverse drug events. That’s more than car accidents or falls among older adults.
Which Drugs Are Most Dangerous?
Not all medications carry the same risk. Some are far more likely to cause harm. According to global data, antibiotics are the top offender, responsible for about 20% of all medication-related harm. Why? Because they’re overused, misprescribed, or taken incorrectly. People stop taking them early when they feel better, or they take leftovers from a previous illness. Both are dangerous.
Antipsychotics come in second at 19%. These are often prescribed to older adults with dementia, even though they can increase the risk of stroke and sudden death. In Australia, efforts to cut down on these prescriptions led to an 11% drop in dispensing for seniors between 2016 and 2021. That’s progress-but it’s still happening.
Central nervous system drugs (16%) and cardiovascular medications (15%) are also high-risk. Blood pressure pills, diabetes drugs, and heart medications require precise dosing. A small mistake can lead to a fall, a stroke, or organ failure. And don’t forget IV medications-these have error rates between 48% and 53% in hospitals. One wrong drop of fluid can change everything.
What’s Happening at Home?
Most medication mistakes don’t happen in a hospital. They happen in your kitchen, your bathroom, or your bedroom. Studies show that between 2% and 33% of patients make errors at home. That wide range? It’s because some people are careful, and others are overwhelmed.
Here’s what goes wrong:
- Taking the wrong dose (too much or too little)
- Missing doses or taking them at the wrong time
- Not finishing a full course of antibiotics
- Mixing pills with alcohol or other meds without knowing the risks
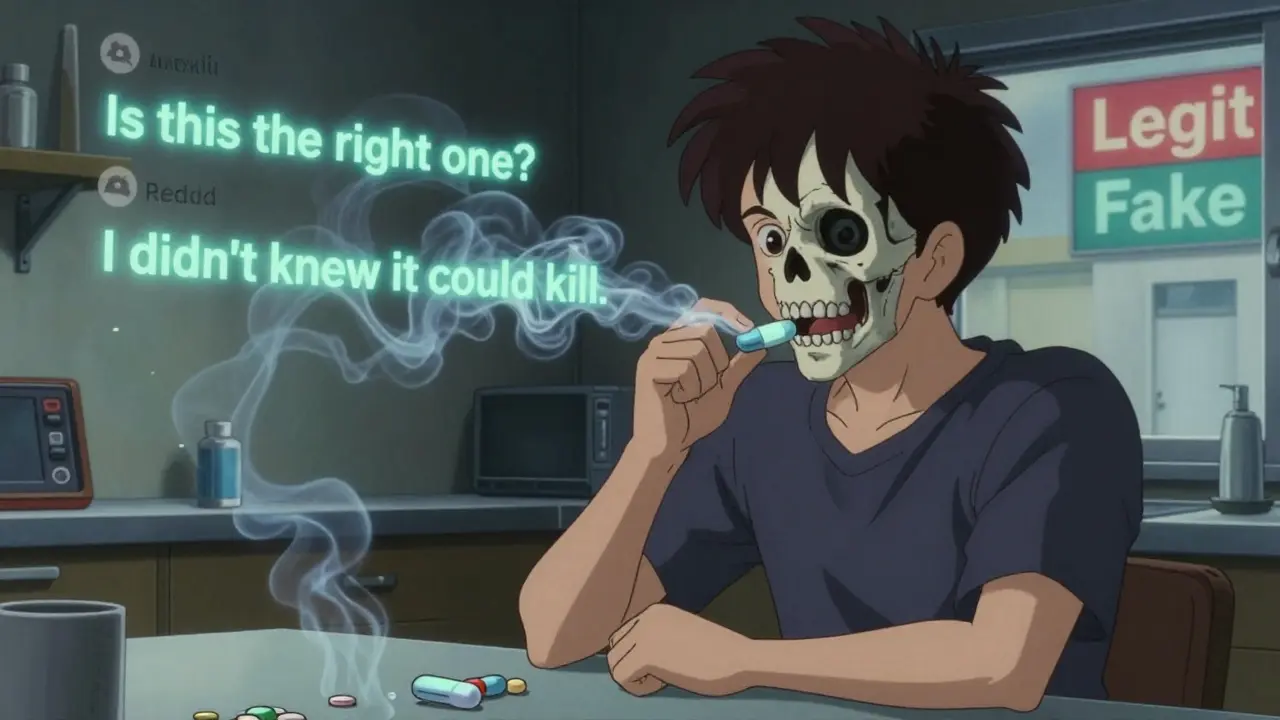
Reddit threads from the r/meds community in early 2025 showed that 68% of questions from patients were about confusion over dosage instructions. Another 22% were about side effects no one explained. If you’ve ever stared at a pill bottle thinking, “Is this the right one?”-you’re not alone.

The Fake Drug Crisis
Online pharmacies are growing fast. So are fake pills. The DEA seized nearly 10 million counterfeit pills between January and September 2021. By 2023, they seized over 80 million fentanyl-laced tablets. Fentanyl is 50 to 100 times stronger than morphine. A single pill can kill. And many of these pills look exactly like legitimate oxycodone or Xanax.
One in three fake drug seizures in the world happens in North America. The DEA says fentanyl is now the leading cause of death for Americans aged 18 to 45. It’s not just a street drug problem-it’s a pharmacy problem. People buy pills from social media sellers who claim they’re “prescription strength” or “safe.” They’re not. They’re poison.
The European Union and Australia have responded with strict packaging rules and real-time prescription tracking. The U.S. is catching up, but the damage is already here.
Who’s Most at Risk?
Older adults are the most vulnerable. People over 65 take an average of four prescription drugs daily. That’s a lot of pills, a lot of chances for error. In Australia, 11% fewer antipsychotics were prescribed to seniors between 2016 and 2021. That’s a win. But many still get drugs that shouldn’t be used in their age group.
Children are also at risk. A child given an adult dose of acetaminophen can suffer liver failure. A teenager misusing Adderall for studying can develop heart problems or addiction. And people with chronic illnesses-diabetes, heart disease, HIV-are often on complex regimens. One missed dose can undo months of progress.
Low-income patients, non-English speakers, and those without regular access to a pharmacist are at higher risk too. If you can’t afford a pharmacy visit or don’t have someone to explain your meds, you’re more likely to make a mistake.
What Can You Do?
You can’t control the hospital system. But you can control what happens in your hands. Here’s how:
- Keep a living list of all your meds. Include prescriptions, over-the-counter pills, vitamins, and supplements. Update it every time your doctor changes something.
- Use one pharmacy. It sounds simple, but it’s powerful. One pharmacy can check for dangerous interactions. Multiple pharmacies? That’s a recipe for errors.
- Ask three questions every time you get a new drug: What is this for? How do I take it? What side effects should I watch for? If the answer is vague, ask again.
- Check the pills. If your pill looks different than last time, ask why. Color, shape, or markings can change-even if the name is the same.
- Never share pills. A pill that helps your friend’s anxiety could kill you.
- Use pill organizers. Especially if you take multiple meds daily. A weekly tray with alarms helps prevent missed or double doses.
Australia’s “5 Moments for Medication Safety” is a smart framework:
- When starting treatment
- When adding a new drug
- During hospital transfers
- When managing high-risk drugs
- When reviewing your meds regularly
Use these moments as checkpoints. Don’t wait for a crisis.
The Bigger Picture
Most errors aren’t because someone was careless. They’re because systems are broken. Dr. Donald Berwick, a top patient safety expert, says: “Most medication errors are system failures-not individual failures.” That means blaming a nurse or doctor doesn’t fix the problem. We need better technology, clearer labels, smarter alerts, and more time for pharmacists to talk to patients.
The global market for patient safety tools is growing fast-projected to hit $14.3 billion by 2029. AI-powered tools are being developed to catch errors before they happen. One study says AI reconciliation tools could reduce mistakes by 30% by 2027. That’s promising. But until those tools are everywhere, you’re still your best defense.
Final Thought
Medication safety isn’t about trusting doctors. It’s about partnering with them. You don’t need to be a medical expert. You just need to be informed. Ask questions. Keep records. Speak up. Your life might depend on it.
How common are medication errors globally?
Globally, about 1 in 20 patients (5%) experience avoidable harm from medication each year. This translates to millions of people annually, with an estimated cost of $42 billion USD per year in healthcare expenses.
What types of drugs cause the most harm?
Antibiotics cause the highest proportion of medication-related harm (about 20%), followed by antipsychotics (19%), central nervous system drugs (16%), and cardiovascular medications (15%). Intravenous drugs have the highest error rates in hospitals, ranging from 48% to 53%.
Can fake medications really kill you?
Yes. Fake pills, especially those laced with fentanyl, are a leading cause of overdose deaths. In 2023, the DEA seized over 80 million counterfeit tablets containing fentanyl. These pills look identical to legitimate prescriptions but can be lethal even in tiny amounts.
What should I do if my pill looks different?
Always ask your pharmacist. Pill appearance can change due to different manufacturers or generic switches-but you should never assume it’s safe. Verify the name, dose, and purpose before taking it.
Why is it dangerous to take someone else’s prescription?
Prescriptions are tailored to an individual’s health history, weight, allergies, and other medications. Taking someone else’s drug-even if it’s for the same condition-can cause severe side effects, dangerous interactions, or even death.
How can I reduce my risk at home?
Use one pharmacy, keep an updated medication list, ask your pharmacist or doctor about side effects, use a pill organizer, and never skip or double doses without checking first. These simple steps cut your risk significantly.